Section 1: Lyme Disease and Tick-Borne Illness Overview
ASPIRE talks with Tom Moorcroft, DO about some of the most frequently asked questions on Lyme disease and tick-borne illness including Bartonella and Babesia. This article is divided into 4 separate sections.
- Section 1: Lyme Disease and Tick-Borne Illness Overview
Why Education about Lyme and Tick-Borne Illness is Crucial
Tick-Borne Illness Cases Per Year & Why Education Matters
- 300,000 Cases Per Year of Lyme Disease roughly
- 400,000 Cases Per Year of Tick-Borne Illness roughly
- Lyme disease is 5-6 times more common than HIV/AIDS
- Education will help people get treated more quickly
- Quicker treatment can lead to improved outcomes.
- Education helps people take prevention seriously, so we reduce the number of people infected.
According to the CDC, Lyme disease is the number one vector-borne illness in the United States. The CDC believes their typical numbers are underestimating the number of Lyme disease cases in any given year by a factor of 10. So what does this mean for you and me? It means that when they’re reporting 30,000 cases, it’s probably more like 300,000 cases per year. When they’re reporting 36,000 cases in a year, their research suggests that it’s more accurately closer to 360,000 new cases. Because this is the case, according to the CDC’s own research, Lyme disease is five to six times more common than HIV AIDS. This is a staggering number.
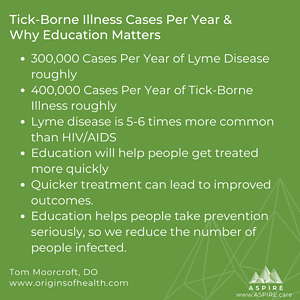 Education is critical to know what is out there. If we can identify cases of Lyme disease early, we can treat them right away. Then we decrease the likelihood of an infection leading to chronic infection and symptoms. We also can bring those numbers down. Awareness and education are really critical; we can actually prevent Lyme and other tick-borne diseases.
Education is critical to know what is out there. If we can identify cases of Lyme disease early, we can treat them right away. Then we decrease the likelihood of an infection leading to chronic infection and symptoms. We also can bring those numbers down. Awareness and education are really critical; we can actually prevent Lyme and other tick-borne diseases.
When we think that there are only 36,000 cases per year, it’s easy to say, “Hey, maybe it won’t affect me.” But when it’s closer to 360,000 cases per year, and it happens to be really common in the state where you’re living, then that’s the time to start thinking, “I need to take this prevention seriously.” This is why education is so important.
How Many People are Infected by Tick-Borne Disease Annually?
There are 360,000 new cases of Lyme disease every year, not including the number of cases of anaplasmosis, ehrlichiosis, Rocky Mountain Spotted Fever, Babesia microti, Babesia duncani, Borrelia miyamotoi, and a few other much less common ones. Lyme disease is by far the biggest piece of that puzzle. Then you add in other infections from the deer tick and other ticks, and the numbers are even higher.
It is important to focus on those Lyme disease numbers. When you look at the infectivity rate of a deer tick, most of that rate is from Lyme disease; Babesiosis is found in 8%, and Borrelia miyamotoi and anaplasmosis are found in around 3% of the ticks infected.
The numbers may be closer to 400,000 a year for all of our tick-borne illnesses. Perhaps even a little bit higher.
Tick Basics
Where Do People Get the Tick Bites? In the deep woods? In their yards?
Where Ticks Live Most
Tick Habitat
- Lyme disease is Para-Domestic
- They live in the Edge – 10’ into the woods & 10’ into the yard
The deer tick is an edge species. The Edge is the area between the yard and the woods if you happen to have that. In a park, there is the open grassy area with wooded areas; The Edge is about 10′ into the woods and 10′ into the grass. There’s approximately a 20-foot border around the edge/the border between the grass and the woods. If you build a garden, about 10 feet into your garden and 10 feet onto your lawn is going to be this hot spot area referred to as the Edge. This is really critical because Lyme disease what’s called para-domestic, which means that 75% of the people are going to get Lyme in a yard. People do not necessarily get Lyme disease when they are hiking in the deep woods; they are coming in contact as they are entering/leaving the deep woods, again, in the edge area.
So with this knowledge, think to yourself, “I’m going walking in this area in the meadow with this groomed trail through the middle, and then we have these tall plants and grasses which is prime tick habitat.” Think about areas where you see deer, mice, and chipmunks; this is going to be the area you see ticks. Keep this in mind when you’re planning the lay out of your yard. If you have a swing set, don’t put it in the shade next to the woods. Move it out, so it is in the sun. You may have to wear hats, longer clothes, and some sunscreen, but you are not playing in the Edge. Another thing to consider is how much garden, do we really want? I’m not saying, don’t have a garden. When you’re out in your garden, you need to know this is an area where ticks could be. We have to take the utmost precautions when playing in our yards.
Don’t be afraid of yards or the deep woods; just be knowledgeable. We can learn how to prevent it when we know more about being exposed.
Lifecycle, Attachment & Transmission Time
Do Ticks Transmit Lyme Disease in All Lifecycle Stages and Which Stage Transmit Most Often?
Tick Stages & Transmission
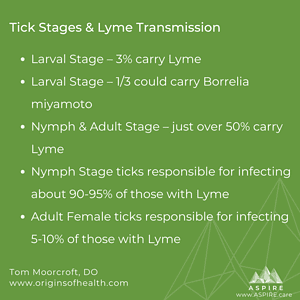
- Larval Stage – 3% carry Lyme
- Larval Stage – 1/3 could carry Borrelia miyamoto
- Nymph & Adult Stage – just over 50% carry Lyme
- Nymph Stage ticks responsible for infecting about 90-95% of those with Lyme
- Adult Female ticks responsible for infecting 5-10% of those with Lyme
The larva, as it just hatched, only have a 3% chance of carrying Lyme disease. Every once in a blue moon, there will be transmission trans-ovarially – meaning from mom to babies. Typically the larva has a blood meal, which is when it can get infected, then evolves into the nymph stage. In the larval stage, Borrelia miyamoto might be in a third of the ticks. The larva is not typically feeding on people, which lowers our risk of being infected during that stage.
The nymph and adult stages are when ticks are infected. Ticks in the nymph stage infect are responsible for 90-95% of the cases of Lyme disease. These are the ones we worry about the most. The reason is probably that they are the size of a 12 point font period, or the size of a poppy seed. Nympha ticks are going to be in protected, humid, warm dark places. It is crucial to do full tick checks, including the groin, under the armpit, the ears, or in the hair. Know they are tiny and might not be a new freckle. I haven’t seen any research indicating the nymph is more virulent than the adult. The adult female, which is responsible for the other 5-10% of cases, has an orangish-red backend.
Tick Attachment & Transmission Times
- Not accurate – 36 to 42 hours of attachment for transmission of Lyme
- Cases show transmission of Lyme in less than 24 hours.
- Around 24 to 36 hours, the likelihood of transmission begins to increase dramatically
- Anaplasma can be transmitted in as little as 8 hours
- If an infected nymph is attached for 4 days, the likelihood of transmission is over 95%
Most information on attachment and transmission is based on data for the deer tick. The information we see the most says attachment needs to be 36 to 42 hours before transmission; this is not completely accurate.
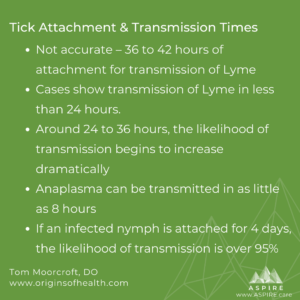 What is accurate is that around 24 to 36 hours, the likelihood of transmission begins to increase dramatically. But we know Lyme can transmit within the first 24 hours of attachment as supported by several cases in the medical literature. I’ve submitted cases for publication confirming this, and the editors said the information sounded scientifically reasonable and valid, but the readers of the journal would not be interested in knowing that information. This is censorship in the medical literature. What we need to be able to do is put information in the literature and talk about whether it’s important rather than the editor determining it. The literature shows that Anaplasma can be transmitted in as little as eight hours after attachment.
What is accurate is that around 24 to 36 hours, the likelihood of transmission begins to increase dramatically. But we know Lyme can transmit within the first 24 hours of attachment as supported by several cases in the medical literature. I’ve submitted cases for publication confirming this, and the editors said the information sounded scientifically reasonable and valid, but the readers of the journal would not be interested in knowing that information. This is censorship in the medical literature. What we need to be able to do is put information in the literature and talk about whether it’s important rather than the editor determining it. The literature shows that Anaplasma can be transmitted in as little as eight hours after attachment.
A nymph will feed for four days. An adult will feed for five days. In the first 24 hours, the infectivity rate is low, then as you get into day two and three and four, it begins to rise exponentially. If an infected nymph is attached for four days, the likelihood of transmission is over 95%. The same stats hold true if you spread that out over five days with an adult. Unfortunately, this is why some say a tick has to be on for a day and a half or two days, or it doesn’t count. Well, that’s crazy because we know that it can be transmitted within the first day.
How Tick-Borne Infections are Transmitted
Transmission of Tick-Borne Infections
- Spirochetes live in mid-gut of tick
- Spirochetes must swim up the digestive track to transmit
- Mouthparts are barbed so enter easily but are not removed easily
- Ticks inject an anticoagulant to allow blood to flow
- Ticks inject an anesthetic so you don’t feel it
The spirochete lives in the tick’s mid-gut, like its stomach, and it has to swim up the digestive tract, and then get into you. But we have found, albeit not often, ticks can have spirochetes in their salivary glands so, theoretically, you can have near instantaneous infection. When the tick bites, it injects an anticoagulant to make the blood flow freely, and an anesthetic so you don’t feel the bite.
Some people will have an itchy reaction to the anesthetic. This itching is similar to when one is given novocaine or lidocaine as a numbing agent. If you happen to be one of those people who react to the anesthetic, you might have a better chance of detecting the tick sooner.
How to Remove Ticks Properly
Tick Removal
- Proper removal may prevent infection
- Do not put anything on the tick: oils, alcohol, etc
- Do not burn it off
- Do not twist
- Do not yank
- Place fine tip tweezers close to skin on mouth part, lift and hold
- Might need to hold up to 2 minutes
- Want tick to back out on its own
- Do not want the tick to regurgitate tick-borne infections into skin
- If mouthpart remains, it is okay
- Clean area after and watch for infection or rash
Removing a tick correctly may prevent being infected by the tick.
Never put essential oils on it, rub it with alcohol, burn it off, just yank it off, or twist it off. It is important to understand how the tick attaches to its host and how that impacts proper removal. The tick’s mouthparts are barbed, almost like a fishhook, with reverse curves, so they get in but are really hard to get out.
Get really fine tip tweezers or maybe one of those v tick removers. Place the tweezers right next to the mouthparts, which is close to the skin as possible. Do not rip out because that can leave mouthparts in the skin and cause a secondary infection. Next, lift and hold; give the tick time to back out naturally. This could take 10-30 seconds or even 2 minutes. Lift, hold, and wait; let it come out on its own. If you put ointments on it or crank it up with a twist, you will potentially irritate the tick, making it want to get out quickly, which at that point, it regurgitates to jet propulsion itself out. We don’t want it to vomit its stomach contents where the Lyme spirochete is primarily held. Now, if you lift and hold but a little part of the mouthparts stays in, that’s fine. If you can get the mouthpart out, great, otherwise clean it off really well and keep an eye on it. The goal is to get the tick out in the least traumatic way to the tick, and ourselves, to minimize the risk of additional transmission.
Ticks & Common Infections They Carry – Lyme & Co-Infections
- Common Ticks – Deer, Dog, Lone Star, Wood, Gulf Coast
- Deer tick carry – Lyme, Babesiosis, Anaplasma, Borrelia miyamotoi, Powassan Virus, Tick-Borne Relapsing Fever
- Dog tick carry – Rocky Mountain Spotted Fever, Tularemia
- Lone Star tick carry – Ehrlichia, Rocky Mountain Spotted Fever, ‘Stari’ borreliosis
- Ticks can transmit more than one agent in a single bite
Do we have to worry about all ticks or just deer tick?
Deer ticks from the East Coast are Ixodes scapularis, and those on the West Coast are Ixodes pacificus. Some of the other common ticks are the Dog, Lone Star, Wood, and Gulf Coast. All can carry different pathogens. The Dog tick can carry Rocky Mountain Spotted Fever, which can be life-threatening, if not identified and treated quickly. You could get tularemia from a Dog tick bite, although it’s very uncommon. The Lone Star tick, with the big white splotch on its back, can transmit Ehrlichia. Ehrlichia, like Rocky Mountain Spotted Fever and Anaplasma, can cause acute symptoms such as fatigue, muscle pains, general malaise, sometimes “ice pick” type headaches and fevers, but could occasionally be life-threatening. It does happen; whenever we’re having acute fevers and headaches after a tick bite, we need to be aware of that. You can get other illnesses from Lone Star ticks, but they are much less common.
What Other Infections do Deer Tick Transmit?
The common infections are Babesious, Anaplasma, and Borrelia miyamotoi, a Lyme-like spirochete infection that causes some symptoms similar to Lyme disease.
Borrelia miyamotoi, in the Relapsing Fever Borrelia group, has a hodgepodge of all the symptoms from other ticks. It’s really confusing at times because you could get 1, 2, 3, or 4 infections from a deer tick. Then you wonder if it is Lyme or Borrelia miyamoto, as both can cause an erythema migrans rash, fevers, headaches, and sweat. Or is it Babesia, Lyme, and Anaplasma?
Powassan Virus (PWV) is a virus you can get from a deer tick. It is not as common as Lyme disease or Babesiosis, but it causes significant illness. Again, its symptoms look like some of the other ones. Powassan Virus can cause some longer-term issues if not caught early on, or if it gets to the severe stages. About half of the people with late-stage PWV disease develop ongoing problems, including cognitive decline and the potential for other neurologic problems. PWV testing is not as readily available; it can be done. The results are not back quickly, and we don’t have a treatment for it right now. Treatment is based on a supportive care model; we try to make you feel good as you can while you get through it.
If you get bitten by a deer tick and testing is negative, we have to think about whether it is PWV or is it more likely to be Lyme. Lyme can look like an acute viral illness; it’s often called summer flu. We have to consider what infection it is most likely to be and consider what other infections it could be. I know that I can treat Lyme disease as well as Borrelia miyamotoi and Anaplasma with the same treatment if I choose my treatment properly. Then I can keep an eye out for Babesia specific symptoms. And after treating those illnesses, but some symptoms remain, it may be PWV. We have to look at the numbers and ask what is most likely, which is Lyme.
Can a Tick Transmit More Than One Infection in a Single Bite?
Yes. A deer tick can carry and transmit multiple bacteria in a single bite.
See Article: Polymicrobial Nature of Tick-Borne Diseases
About the Erythema Migrans Rash
What Percentage of People an Erythema Migrans Rash?
- The rash is pathognomonic for Lyme disease. A negative test, along with the rash, does not negate a positive diagnosis.
- CDC says 70% get the erythema migrans rash
- Literature says 40-60% get the erythema migrans rash
- Only 20-30% of erythema migrans rash are bullseye rashes
- 70-80% of erythema migrans rashes are circular or ovoid but can be big splotches. Can be red or purple.
- 200mg of doxycycline if given right after tick bite may prevent the rash but won’t cure Lyme disease and may cause a false negative on testing. The study that says 200mg of doxycycline cures Lyme is flawed.
According to the CDC, about 70% of people have this erythema migrans rash. But the medical literature shows a rate of 40 to 60%. Basically, there is a 50/50 chance. Clinically, those who treat a lot of Lyme disease feel the percentage is a lot less.
The rash is pathognomonic for Lyme disease. If you have this rash and you live in an endemic area for Lyme, which is most of the United States, you do not need to do any further Lyme testing. But you might want to test for co-infections. If you have the rash and do a Lyme test, but it comes back negative, the test does not negate the fact that you have Lyme disease.
Are All Erythema Migrans Rashes a Bullseye Rash?
No. The bull’s eye rash is a type of erythema migrans rash. Bullseye rashes only count for about 20% to 30% of the Erythema Migrans rashes. The bullseye rash has a little central clearing, then a red ring, then a clear ring, and then some additional redness.
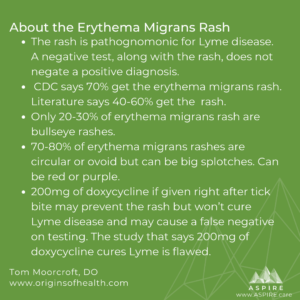 However, the erythema migrans rash is most commonly a big, blotchy red rash. It is typically circular but sometimes ovoid. Sometimes it looks like a dark purple or red blotch. Just because it doesn’t have this ringed appearance, doesn’t mean it’s not erythema migrans. The bottom line is that not all erythema migrans rashes look like a bullseye, and not all people who have Lyme disease get any rash.
However, the erythema migrans rash is most commonly a big, blotchy red rash. It is typically circular but sometimes ovoid. Sometimes it looks like a dark purple or red blotch. Just because it doesn’t have this ringed appearance, doesn’t mean it’s not erythema migrans. The bottom line is that not all erythema migrans rashes look like a bullseye, and not all people who have Lyme disease get any rash.
In terms of prevention of Lyme disease following a tick bite we do not have much good data. There is one study commonly cited to guide clinical practice, however it is flawed. It says a double dose of doxycycline, after a tick bite, will prevent Lyme disease. This is not accurate. We found in the study that 200 milligrams of doxycycline may prevent you from getting a rash. But, the study was not designed in a way to say this prevented Lyme disease. A small dose may actually inhibit proper antibody production leading to a false negative test result. So essentially, that small dose may take away the possibility of having the rash, and thus a definitive diagnosis. It could interfere with your ability to make proper antibodies to give you a positive on a lab test that would also help make a diagnosis.
See photos of the Erythema Migrans Rash.
Do Children and Adults Get the Same Lyme Disease Symptoms?
- Common in Adults – Classic Lyme symptoms: fatigue, joint pain, “summer flu”
- Children can have common symptoms but they can have GI problems with no other explanation
- Children can have regression – behaviorally, cognitively and PANS symptoms See PANS Symptoms
The classic Lyme disease symptoms of fatigue, joint pain, and summer flu symptoms are much more common in adults than kids, but kids can still get them. With kids, you have to be concerned about gastrointestinal problems that have no better explanation, including just pain and sometimes food allergies, especially in conjunction with summer flu symptoms. We often will see a regression in children – particularly mental and emotional regression. Before they’re doing well in school, reading at grade level and now they’re reading at three grade levels below. We can also see changes in penmanship and drawing ability. Additionally, there can be focus issues and behavioral regression; children start behaving like a toddler, but they’re 10. Kids can have rage, OCD, and anxiety that is not a result of a currently stressful situation.
Section Links to Overview of Lyme & Tick-Borne Illness – Dr. Moorcroft
- Section 1: Lyme Disease and Tick-Borne Illness Overview
- Section 2: Treatment for Lyme Disease
- Section 3: PANS & Lyme Disease
- Section 4: Bartonella & Babesia Co-Infections