PANS & Eating Disorder/Food Restrictions & Toolkits/Handouts
PANS PANDAS & Eating Disorders/Food Restrictions – Full Packet of Recent studies and Flyer. Please note that the Flyer is also available in two poster sizes...
This is a paradigm shift and a challenge for providers to link the medical history with a sudden change from the baseline of functioning to the acute onset of psychiatric symptoms in a child, especially with the frequent lack of coordination between medical and mental health providers. It truly takes a cross-discipline collaborative effort to identify and most effectively treat PANS/PANDAS. As mental health clinicians, we do not often have the opportunity to be on the prevention side of disorders; with an increase of PANS/PANDAS knowledgeable medical and mental health treatment providers, we can do just that! –Christine Amabile, LCSW, ASPIRE Provider Outreach & School Education Committees
Links to sections within Behavioral Health
Links to other website sections
With PANS PANDAS, the parent is often the driving force to get help in returning their child to normal functioning. Be a partner with the family. The majority of parents are traumatized and need compassion. Providers must validate the parent and child’s experience. It is terrifying and stressful for families to watch these symptoms suddenly occur. They are often at a complete loss about what it is or how to treat it. Then they are too often minimized, dismissed, or rejected by the very medical community that you turn to for help. Informed parents know their children and often cannot convince doctors to acknowledge or treat PANS PANDAS. Have the research and resources ready to assist families in combating any barriers blocking treatment and advocate for the child’s needs.


This chart provides an overview of behavioral interventions for PANS PANDAS. For more detailed information on the three-pronged treatment approach to treating PANS PANDAS and providing symptomatic relief, including behavioral interventions for specific symptoms including Cognitive Behavior Therapy (CBT)/ Exposure Response Prevention (ERP) and using psychoactive medications, please see:
PANS PANDAS & Eating Disorders/Food Restrictions – Full Packet of Recent studies and Flyer. Please note that the Flyer is also available in two poster sizes...
Living with a sibling affected by PANS profoundly impacts well-being—fear of outbursts, limited social opportunities, and the isolation of not having the words or knowledge to explain the...
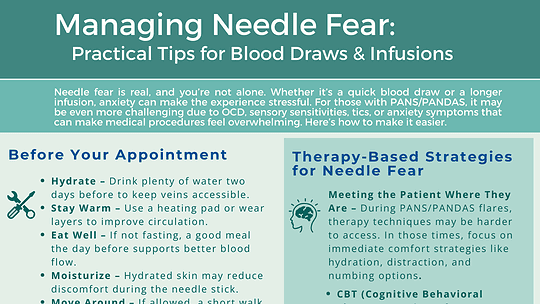
Needle fear is real, and you’re not alone. Whether it’s a quick blood draw or a longer infusion, anxiety can make the experience stressful. For those with PANS/PANDAS, it may...

Clinic Providers & Healthcare Workers – Join Us at the MAPS Spring 2025 Functional & Translational Medicine Conference Register using the ASPIRE discount code and enjoy a 30% discount!...
ASPIRE’S Professional Advisory Board publishes PANS/PANDAS Guidelines for Children with Autism PANS PANDAS & Autism Autism PANS Guidelines Children who have autism spectrum disorder (ASD or...

Shedding Light on the Link Between Self-Harm and Suicidality in PANS and Immunopsychiatric Disorders Gunilla Gerland, former Chair of SANE, has translated their recent white paper on suicidality and...

Speaker: Julie Cox, MSW, LCSW, PLLC Webinar: Helping PANS Families Move From Grief to Empowerment Register to View Recorded Webinar: Watch on Demand Please register even if you will not attend...
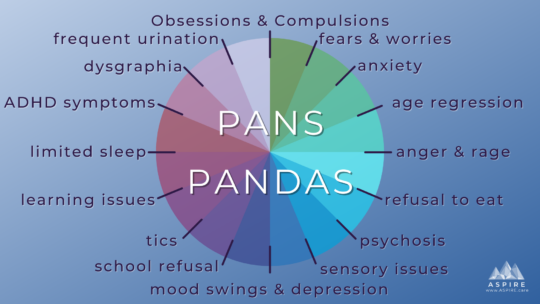
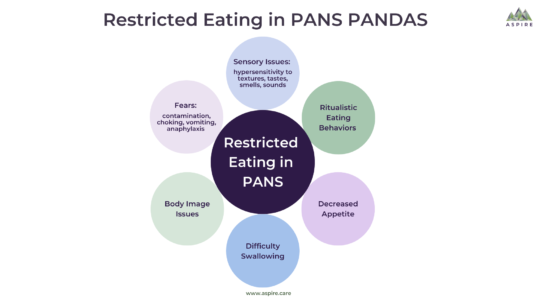
Learn more about PANS PANDAS PANS PANDAS are misdirected immune responses that result in acute onset of OCD, tics, and/or restricted food intake, along with two neuropsychiatric symptoms in seven...
Speaker: Patricia Rice Doran, EdD Webinar: Behavioral Support for Students with PANS PANDAS at School Register for this webinar: Replay Available Soon. Please register even if you will not attend...

Speaker: Peggy Chapman, RN Webinar: Psychiatric Medication Strategies for Children with PANS/PANDAS Date/Time: Monday, June 27 at 6:00 PM EST Register to view webinar: Watch on Demand About this...

Lecturer: Nancy O’Hara, MD, MPH, FAAP Webinar: Demystifying PANS/PANDAS: A Functional Medicine Guide on Basal Ganglia Encephalitis Date/Time: Monday, May 2nd – 4:00 PM EST Register for this...

Lecturer: Susan Swedo, MD Webinar: PANS and PANDAS Recognition, Diagnosis and Treatment of Acute-onset Neuropsychiatric Symptoms Date/Time: Thursday, March 24 To Watch Webinar: Please fill out the...