
Abrupt-Onset Eating Restriction in PANS
Kapphahn C, Peet B, Gao J, Chan A, Farhadian B, Ma M, Silverman M, Tran P, Schlenk N, Thienemann M, Frankovich J. Sudden Onset Disordered Eating Behaviors and Appetite...
PANS Consensus Statement on Diagnosing PANS and PANDAS –Clinical Evaluation of Youth with Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS): Recommendations from the 2013 PANS Consensus Conference. Chang, MD et al (JCAP, Vol 25, No 1, 2015 Mary Ann Liebert, Inc.)
PANS PANDAS Symptoms PANS Consensus Statement
More on the PANS Diagnostic Process
The PANDAS Physicians Network (PPN) flowcharts for diagnosis and treatment will help clinicians evaluate their patients and determine the best course of treatment. Guidelines and workflows were approved by practitioners of the PANDAS Physicians Network Scientific Advisory Board. More detailed resources are available at www.pandasppn.org. Diagnosing and treating should be done by a licensed healthcare provider.
Primary care providers play important, ongoing roles in the diagnosis, treatment, and recovery of children with PANS/PANDAS. Children with a moderate or severe/life-threatening onset or a complex presentation may require treatment by an experienced multi-disciplinary team of specialists or a PANS/PANDAS specialist. Additional resources can be found at
PANS treatment utilizes three complementary modes of interventions to treat the patient completely. Three-pronged treatment protocols are dependent on disease trajectory, symptoms, and severity as well as lab work and patient history.

JCAP PANS Treatment Guidelines
The PANDAS Physicians Network (PPN) flowcharts for diagnosis and treatment will help clinicians evaluate their patients and determine the best course of treatment. The diagnostic flowchart and treatment guidelines include a detailed process provided for determining the appropriate diagnosis and symptom severity-based treatment protocols for mild, moderate, and severe/extreme cases.
Download PPN Treatment Flowchart
 PANS PANDAS Clinician Toolkit
PANS PANDAS Clinician ToolkitThere are invaluable resources to help clinicians learn how to recognize PANS PANDAS symptoms, do a workup to inform a possible diagnosis, and create a treatment plan. ASPIRE has assembled this one-page Clinician Toolkit but there are many resources throughout the website, and we are always adding more. So, check the website often.
 Diagnosis & Treatment of PANS PANDAS – Provider Packet
Diagnosis & Treatment of PANS PANDAS – Provider PacketClick the button below to download the twelve-page information packet Provider Information on PANS PANDAS, including Symptoms, Diagnosis, and Treatment.
 PANS PANDAS Guidelines for Children with Autism
PANS PANDAS Guidelines for Children with Autism
 Testing & Antibiotic Usage for GAS in PANS & PANDAS
Testing & Antibiotic Usage for GAS in PANS & PANDASASPIRE’S Professional Advisory Board Toolkit:
PANS is a clinical condition identified by an abrupt onset of a specific cluster of symptoms as a result of a variety of etiologies and disease mechanisms. Therefore, tracking symptoms, onset, severity, and duration is a critical part of making a clinical diagnosis and forming treatment plans. There are two useful PANS Symptom Rating Scale tools.

Developed by Tanya Murphy, MD and Gail Bernstein, MD. Source: PANS/PANDAS: CLINICAL & RESEARCH UPDATE, Gail A. Bernstein, M.D., 12/9/16, University of Minnesota
You can scroll through the pages of the Clinician Resources below. However, clicking on the link to the main Clinician Resources page is easier. Otherwise, you will be redirected to the top of this page each time you scroll to a secondary page in the resources.

Kapphahn C, Peet B, Gao J, Chan A, Farhadian B, Ma M, Silverman M, Tran P, Schlenk N, Thienemann M, Frankovich J. Sudden Onset Disordered Eating Behaviors and Appetite...
Wu, X., Hao, J., Jiang, K. et al. Neuroinflammation and pathways that contribute to tourette syndrome. Ital J Pediatr 51, 63 (2025). https://doi.org/10.1186/s13052-025-01874-3 A 2025 narrative review...
Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS) is a neuropsychiatric syndrome that develops after a Streptococcus pyogenes (group A strep)...
Occupational Performance Fluctuates With PANS Disease State Newby MJ, Lane SJ, Haracz K, et al. Occupational performance patterns in children with paediatric acute-onset neuropsychiatric syndrome....
Arthritis in Children with Psychiatric Deterioration: What This Case Series Shows Ma M, Sandberg J, Farhadian B, Silverman M, Xie Y, Thienemann M, Frankovich J. Arthritis in Children with Psychiatric...
When PANS and IBD Co-Occur: What This Case Series Suggests Tang AW, Swedo SE, Pasternack M, Murphy T, et al. Eight cases of pediatric acute-onset neuropsychiatric syndrome: clinical characteristics....
In this study, neurological soft signs (NSS) are defined as subtle neurological examination findings that may reflect dysfunction in motor coordination and movement regulation, particularly related...
Children and adolescents typically experience mild or asymptomatic acute COVID-19. However, a significant subset develop persistent symptoms, commonly termed long COVID or post-COVID condition....
Fidan T, Ceyhan S, Fidan V. Streptococcal Serology in Children With Stuttering. Ear, Nose & Throat Journal. 2024;104(8):513-515. April 19, 2024. doi:10.1177/01455613241244946 Stuttering and...
Association of PANS With Microstructural Brain Differences on Diffusion MRI Study: Zheng J, Frankovich J, McKenna ES, et al. Association of Pediatric Acute-Onset Neuropsychiatric Syndrome With...
By Gabriella True, President, Alliance to Solve PANS & Immune-Related Encephalopathies (ASPIRE) Each year, countless children and adults with PANS PANDAS lose critical time, time when early...
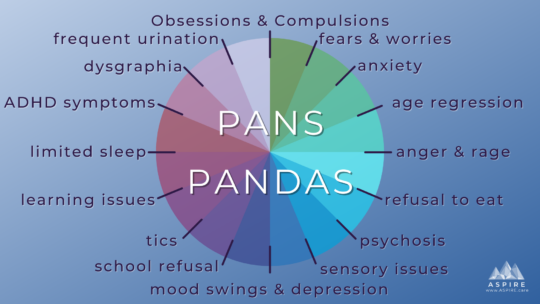
Learn more about PANS PANDAS PANS PANDAS are misdirected immune responses that result in acute onset of OCD, tics, and/or restricted food intake, along with two neuropsychiatric symptoms in seven...