PANS treatment utilizes three complementary modes of interventions to treat the patient completely.
Treating PANS PANDAS
General Overview
The PANS/PANDAS Research Consortium (PRC) published PANS PANDAS Treatment Guidelines in the Journal of Child and Adolescent Psychopharmacology (JCAP Vol. 27 #7, 2017). Below is a summary of these guidelines; please read the published guidelines for specifics on medications, dosages, side effects, pertinent studies, and complete citations. The PANDAS Physicians Network (PPN) flowcharts for diagnosis and treatment will help clinicians evaluate their patients and determine the best course of treatment. Diagnosing and treating should be done by a licensed healthcare provider. Primary care providers play important, ongoing roles in the diagnosis, treatment, and recovery of patients. Patients with a moderate or severe/life-threatening onset or a complex presentation may require treatment by an experienced multi-disciplinary team of specialists or a PANS/PANDAS specialist.
ASPIRE Clinician Toolkit PPN Diagnostic & Treatment Flowchart
“At A Glance” – Treating PANS PANDAS
Three-Pronged Approach
80% of PANS patients present with neuroinflammation and/or postinfectious autoimmunity. Consequently, PANS treatment utilizes three complementary interventions to treat the patient completely. Doctors must individualize treatment protocols according to the patient’s severity of symptomology, course of illness, lab testing, and physical exam. Primary care providers can treat most PANS patients with the direction of the Treatment Guidelines. However, clinically complex patients may require a team of PANS clinicians.

(Overview of Treatment of PANS, Swedo, MD et al, JCAP-Vol27, #7, 2017)
Treating of PANS PANDAS involves a three-pronged approach that utilizes psychiatric medications when appropriate to provide symptomatic relief, antimicrobial treatments to eliminate the source of neuroinflammation, and anti-inflammatory and immune-modulating therapies to treat disturbances of the immune system.”
- Treat Symptoms: psychoactive medications, psychoactive therapies, and supportive therapies
- Remove Inflammatory Source: antimicrobial treatments
- Treat Immune System Dysregulation: anti-inflammatory and/or immunomodulating medications
“At A Glance”
Treatment Basics

Symptoms Treatment
- Cognitive Behavior Therapy (CBT)
- Psychotropic Medications: “start low & go slow’’ approach
Inflammatory Source Treatment
- Antimicrobial Treatments: Therapeutic or prophylactic antibiotics
- Other medications like anti-virals if the trigger is not a bacterial infection
Immune System Dysregulation Treatments
- Anti-Inflammatories: NSAIDs, Corticosteroids
- Intravenous Immunoglobulin (IVIG)
- Plasmapheresis (PEX)/ Therapeutic Plasma Exchange (TPE)
- Rituximab, Cellcept, and other immunomodulatory agents
Other Treatment Options
- Tonsillectomy and Adenoidectomy
- Antivirals
- Antifungals
- Antihistamines (H1 & H2 Blockers)
- Vitamin D3, Omegas, etc
- Dietary Changes
“At A Glance”
Guidelines for Treating PANS PANDAS
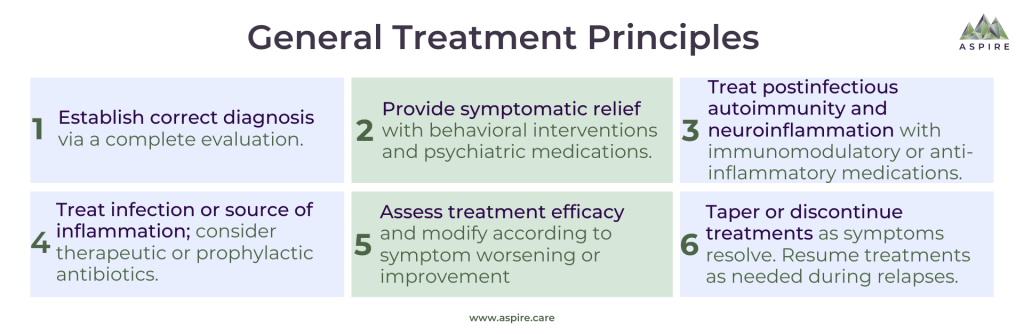
Establish Correct Diagnosis
Properly establish PANS PANDAS is the accurate diagnosis via a complete evaluation. PANS PANDAS is a clinical disorder and a diagnosis of exclusion defined by abrupt onset of obsessive-compulsive symptoms and/or severe eating restrictions and at least two concurrent cognitive, neurological, or behavioral symptoms.
Provide Symptomatic Relief
Provide symptomatic relief with behavioral interventions and psychiatric medications. Prioritize treatments based on which symptoms are the most immediately concerning. Treatments must be individualized and will require adjustment over time. Patients with mild to moderate symptoms may not require any pharmacological intervention. Psychiatric medications generally should be implemented with a ‘‘start low & go slow’’ approach. PANS patients may not be able to participate in CBT due to overwhelming symptoms during the acute stage of illness. However, caregivers should begin instruction on behavioral interventions to learn how to manage symptoms at home.
Treat Postinfectious Autoimmunity and/or Neuroinflammation
An Immunomodulatory treatment plan is based on disease trajectory and symptom severity; it must be an individualized protocol. Immune treatments are used only in PANS patients demonstrating signs of postinfectious autoimmunity and/or neuroinflammation, which are seen in at least 80% of patients. Guidelines for treating postinfectious autoimmunity and/or neuroinflammation in PANS are predicated on decades of treating other neuroinflammatory disorders and postinfectious autoimmune conditions.
Treat Source of Infection
For PANS PANDAS flares triggered by an infection, treat the underlying infection thoroughly. While GAS is the most studied inciting infection, there are many other infections known to trigger PANS flares such as various upper respiratory tract infections, Mycoplasma pneumoniae, influenza, etc. Even without a documented infection, a course of antibiotics is suggested at the time of diagnosis. Extended and/or prophylactic courses of antibiotics should be considered for strep-triggered PANS/PANDAS.
Assess Treatment Efficacy
When treating PANS PANDAS, periodically assess the efficacy of treatment protocols. Modify the plan according to symptom worsening or improvement
Taper/Cease Treatment
As symptoms resolve, taper or discontinue interventions. Treatments may need to be resumed, as PANS is often relapsing-remitting. PANS PANDAS can be relapsing-remitting, chronic-static, or chronic-progressive.
Three-Pronged Approach Treatment Strategies
Three-pronged treatment protocols are dependent on disease trajectory, symptoms, and severity as well as lab work and patient history.
-
Provide Symptomatic Relief
-
Treat Postinfectious Autoimmunity and/or Neuroinflammation
-
Treat Source of Infection
 Provide Symptomatic Relief
Provide Symptomatic Relief
PANS/PANDAS treatment is a three-pronged strategy; treat PANS PANDAS symptomatically while treating inflammation, immune system, and infections. Prioritize the behavioral, and psychiatric treatments based on which symptoms are the most immediately concerning, and creating the most interference. Treatments must be individualized and will require adjustment; symptomology and severity differ per child. Psychiatric medications, generally, should be implemented with a ‘‘start low & go slow’’ approach; beginning dosages for PANS PANDAS are typically ¼ or less typical doses. Patients with mild to moderate symptoms may not require any pharmacological intervention while those with more severe symptoms may require behavioral therapy, further education, and pharmacologic treatments. Treatments should be reviewed periodically and adjusted as per symptom severity; symptoms can change during a flare and from flare to flare. The disease trajectory and the efficacy of other treatments such as antibiotics, anti-inflammatories, and immunomodulators vary from patient to patient. Some patients react positively and quickly to medical interventions, while others experience less positive outcomes. Thus, mental health providers are advised to not always make quick changes with every symptom change. See more on Behavioral Health.
Cognitive Behavior Therapy (CBT)/ Exposure Response Prevention (ERP)
CBT, when caregivers reinforce it in the home, is the most effective treatment for pediatric OCD. Often the patient is not ready to undergo CBT therapy themselves until medical treatment is well underway and producing favorable results. Thus, caregivers are encouraged to seek out the help of a CBT therapist immediately to learn techniques on how to not encourage OCD rituals and other behaviors, and setting limits while reinforcing good habits. Therapists can assist caregivers in finding ways to reduce unsafe episodes, such as limiting transitions, sensory overload, stressful situations, too many expectations, etc. During unsafe episodes, due to compulsions, and rages, the primary goal of any intervention is to keep the patient safe. Once that episode is over, caregivers are encouraged to resume the tools learned from the therapists. Utilizing CBT tools to minimize and discourage obsessions and compulsions in the home can help prevent them from getting worse and reduce stress in the long run.
Behavioral Interventions
| OCD |
|
| Anxiety |
|
| Depression (Not Severe) |
|
| Tics |
|
| Irritability & Aggression |
|
Psychoactive Medication
Controlled studies have not been done on psychoactive medications and PANS patients. However, clinical experience shows, with careful management, the same medications used for the individual symptoms can be beneficial. Clinicians believe most PANS patients are more prone to have adverse reactions to medications. It is crucial to “start low and go slow”; the general advisement is to begin doses at ¼ or even less of typical starting doses and slowly taper the dose up. Two factors make PANS patients clinically complex, which ultimately increases the difficulty in understanding responses to psychoactive medication:
- Simultaneous multiple symptoms versus “just” anxiety.
- Some medications take days to weeks to take effect, especially with a slow taper, making it hard to discern between reactions, positive or negative, caused by the medications versus those caused by treatments and/or the episodic nature of PANS.
A general, first psychoactive treatment for PANS/PANDAS may be benzodiazepines, which can help alleviate agitation, aggression, anxiety, and insomnia. However, some pediatric patients experience may experience severe disinhibition. Selective serotonin reuptake inhibitors (SSRI) are indicated for some symptoms. Side effects can match the symptoms they are being used for; careful attention must be paid to the timing of symptom change and dosage. Patients placed on antipsychotics should have an EKG before and during treatment to rule out a prolonged QTc.
Inpatient Hospitalization
For patients with dangerous and/or life-threatening behaviors, inpatient hospitalization may be necessary to keep them safe. Ideally, a behavioral unit will have staff qualified to handle medical procedures as well as be trained in behavior modification techniques. Such units are extremely rare; thus, doctors often must choose between a psychiatric unit and a general pediatric hospital.
School Accommodations
Appropriate school accommodations are necessary for most students with PANS/PANDAS. Typically, a 504 plan or an individualized educational plan (IEP) is created. Planning teams should write accommodations based on the student’s worst exacerbation to be appropriately prepared. As PANS symptoms relapse and remit, the school must be able to move the patient in and out of services. Over half of PANS patients miss a significant amount of school. There needs to be a consistent flow of information between the school, its various departments, and the caregivers. School support is part of treating PANS PANDAS. Learn more about PANS at School.
Family Support
PANS places a significant burden on the entire family. Families must remember to take care of themselves. Parents are encouraged to seek local support groups both in-person and online. Parents are also encouraged to find a CBT Therapist to work with to learn tools to incorporate into daily living.
For specific psychiatric and behavioral interventions for each specific symptom (OCD, anxiety, restricted food take, etc.), please refer to Clinical Management of Pediatric Acute-Onset Neuropsychiatric Syndrome: Part I–Psychiatric and Behavioral Interventions, Margo Thienemann, MD et al, Journal of Child and Adolescent Psychopharmacology Volume 27, Number 7, 2017, Mary Ann Liebert, Inc., Pp. 1–8
General Guidelines of Immunomodulatory Therapy for Treating PANS PANDAS
1. New Onset/Acute Flare
- Mild: ‘‘tincture of time’’ along with CBT. If symptoms persist, add nonsteroidal anti-inflammatory drugs and/or short oral corticosteroid bursts
- Moderate-to-Severe: oral or intravenous corticosteroids may be sufficient.
- Extremely Severe: Long, tapered corticosteroid courses or repeated high-dose corticosteroids. TPE is the first-line therapy given with or without IVIG, high-dose intravenous corticosteroids, and/or rituximab.
2. Relapsing-Remitting
- As above
- Look for recurrent or new triggers; treat accordingly
- If immunodeficient, IVIG may be warranted.
3. Chronic-Static or Chronic-Progressive
- Mild-to-moderate and moderate-to-severe symptoms: Prescribe immunomodulatory therapies appropriate to severity
- Severe-to-extreme symptoms: Consider appropriate immunomodulatory therapies. Seek further evaluation.
- Refractory disease course: Seek further evaluation. Consider appropriate immunomodulatory therapies. Consider shifting to primary rehabilitation in cases with possible injured neurocircuitry.
 Treat Postinfectious Autoimmunity and/or Neuroinflammation
Treat Postinfectious Autoimmunity and/or Neuroinflammation
Immune treatments are only used in PANS/PANDAS patients demonstrating signs of postinfectious autoimmunity and/or neuroinflammation, which are seen in at least 80% of patients. Evidence to prescribe these treatments may be obtained from paraclinical assessments, lab work, and physical examination. Immunomodulatory treatment plans are based on disease trajectory and symptom severity; treatment plans must be individualized. The Treatment Guidelines are organized by severity: mild, moderate-to-severe, and extreme/life-threatening clinical presentations. For more information on Symptom Severity. There are supplementary guidelines based on disease trajectory because single disease and relapsing-remitting disease episodes are treated differently than those with a chronic-progressive and chronic-static course.
Overview of Immunomodulatory Therapy Based on Severity & Disease Trajectory for Treating PANS PANDAS
Mild Symptom Severity Treatment
Mild symptoms, once an infection is ruled out or treated, may only need ‘‘tincture of time’’ along with some CBT therapy. However, there may be a relapse. If symptoms worsen or last longer than two weeks, nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended for six weeks. NSAIDs effects can decrease over time, so they should be stopped intermittently; if symptoms return, then another course of NSAIDs should be given. Negative side effects should be watched for, even though two studies reveal no significant toxicities. A recent study reveals that 1/3 of PANS patients improved on NSAIDs and another 1/3 did worse once the NSAIDs were stopped. Another study confirms that NSAIDs are related to shorter flares.
For Mild-to-Moderate Treatment
For mild-to-moderate symptoms, short courses of oral corticosteroids are recommended. Risks are minimal, and if given within the first day of onset, the results can be remarkable. In a recent study, patients with an infectious illness did not have as much benefit from corticosteroids as those without an infectious illness, whose PANS symptoms lasted 6.4 weeks as versus 11.4 weeks. Those with an infectious illness may benefit from a repeated steroid burst if given at symptom onset, or by delaying the initial steroid burst. Patients who relapse or have a prolonged exacerbation may benefit from additional steroid bursts with or without a taper. Caution should be used in patients with rage or aggression as corticosteroids can aggravate these symptoms, but benefits may still outweigh the risks.
Moderate-to-Severe Symptom Severity Treatment
For moderate-to-severe symptoms, immunomodulatory treatments are usually necessary. As with mild symptoms, oral corticosteroids may be adequate if given early. Longer courses equal longer periods of symptom remittance in PANS but risks are increased. Corticosteroids are the standard of care for unexplained new-onset neuropsychiatric symptoms without infections, neurodegenerative disorders, and metabolic disturbances. Patients with chronic-static or chronic-progressive disease see reduced reactions. Due to symptoms returning after the effect of the steroids wears off, IVIG and immunomodulatory agents are often needed. IVIG trials for PANS have only been designed to use a single course of IVIG. However, the PRC members typically use repeated doses on patients who experienced positive results from the first round only to relapse once the IVIG has cleared the system. Since positive results from IVIG often are not seen for 2-3 weeks, additional gains may be seen in each cycle.
Extreme or Life-Threatening Symptom Severity Treatment
For extreme and life-threatening symptoms, TPE is a first-line therapy because it generates the fastest and most significant improvement. TPE will cause hypogammaglobulinemia; clinicians should consider including IVIG in the treatment plan. TPE, on its own, does not produce long-lasting symptom improvements, so a maintenance immunosuppression regimen like rituximab is usually needed. This may be the case in chronic-static or chronic-progressive forms of PANS too. When TPE is not accessible, then IVIG along with IVMP pulses may serve as an alternative. Rituximab or mycophenolate mofetil may be an option in patients with autoimmunity, neuroinflammation or who have relapsed after a period of continued benefit from IVIG or IVMP. Clinicians must be well versed in these treatments. Patients must also be in the care of a psychiatrist who is qualified to manage worsening psychiatric symptoms seen during a treatment protocol.
For additional information on why immunomodulatory treatments are used for PANS, as well as specific considerations and treatment guidelines, see Clinical Management of PANS: Part II—Use of Immunomodulatory Therapies, Jennifer Frankovich, MD, MS, et al., Journal of Child and Adolescent Psychopharmacology Volume 27, Number 7, 2017, Mary Ann Liebert, Inc., Pp. 1–6.
 Treat Source of Infection
Treat Source of Infection
Current data shows that an infection is typically the inciting factor for PANS/PANDAS. As part of the three-pronged treatment approach for PANS, treat the underlying infections thoroughly for all PANS flares triggered by an infection. As indicated by emerging data, the PRC suggests a course of anti-streptococcal antibiotics at the time of diagnosis even without a documented GAS infection. Some patients have reported full recovery due to antibiotic treatment. All PANS/PANDAS patients should be closely examined for intercurrent infections. If positive for an infection, then treat according to standard guidelines.
GAS and PANDAS
40%-77% of PANS cases are associated with strep. The number of prior GAS infections correlates with the severity and frequency of PANDAS flares. The interval between exposure to an infectious organism and the appearance of PANS symptoms ranges from 1 to 3 days prior to strep throat symptoms to 30 plus days post infection.
Not all patients with a GAS infection will present with any GAS infection symptoms. GAS infections do not just occur in the throat; perianal dermatitis is known to trigger PANS symptoms, and impetigo and other forms of the disease are thought to as well. 15% of strep throat cases are missed on rapid strep tests; a culture must be done if negative. The PRC recommends that patients presenting with PANS symptoms be given a throat swab even if no strep throat symptoms are present. The PRC accepts that a 50% fall or rise in ASO and/or ADB titers to be significant. The PRC created guidelines to determine ‘‘adequate’’ or ‘‘not adequate’’ evidence of a past strep infection to diagnose PANDAS.
Antibiotic Treatment for PANDAS
Oral or intramuscular penicillin is the first line antibiotic to treat strep. Injectable antibiotics are used when patients refuse to take medications by mouth. Cephalexin, azithromycin, clindamycin, clarithromycin, and cefadroxil are recommended in patients with persistent or relapsing strep throat, as they may be more effective. Azithromycin may not be effective in some regions of the country but it is effective against mycoplasma and may have immunomodulatory results. Note it should be used with caution in patients with a prolonged QT interval or on medications that cause one like SSRIs.
The PRC recommends ordering a course of antibiotics for a strep infection at the time of PANS diagnosis whether or not a strep infection has been identified. This is similar to the protocol for rheumatic fever. The goal of aggressively treating GAS is to lower the risk of neuronal injury. Some members of the PRC order a 3-week initial dose of an antibiotic to resolve neuropsychiatric symptoms. Although there is not enough data to firmly support long-term prophylactic antibiotic use for PANDAS, one study shows the frequency of GAS infections were reduced by 95%-96% and flares were reduced by 56% to 75% depending on the antibiotic. The PRC commonly order long-term prophylactic antibiotics for strep, especially in patients with severe symptoms and/or frequent PANDAS flares to try and reduce further infections, flares and thus reduce risk of neuronal injury. Guidelines established for the prevention of rheumatic fever are used for PANDAS patients. The precise duration of prophylactic antibiotics has not been established but due to late relapses, it is suggested that one to two years after the last flare may be needed. Patients in remission may be able to cease antibiotics during the summer when exposure is reduced. For severe cases, prophylactic antibiotics may be warranted until 18 years of age depending on severity, relapses, and exposure.
Antibiotic Treatment for PANS
As stated above, even with no signs that strep is the PANS trigger, an initial course of antibiotics is suggested at the time of diagnosis because there may be a hidden infection. Prophylactic antibiotic use is not recommended for patients with no signs of past or current strep infection. Close monitoring of the patient and close contacts is strongly recommended. Siblings between the ages of 3-12 must be especially closely monitored for strep infections and signs of PANS as they have a high genetic risk for having PANS too.
Upper respiratory infections
Upper respiratory infections (common cold, sinusitis, middle ear infections) are associated with the initial onset and subsequent exacerbations of PANS; the specific organism is usually not identified. For acute sinusitis, Amoxicillin-clavulanate (Augmentin) is the preferred antibiotic, especially for those with severe PANS symptoms and/or for patients who have recently been on another antibiotic. For influenza, prevention is key during flu season. Anti-virals for influenza can be used; anti-viral treatment for children can be given after the first 48 hours of illness as they may shed the virus for longer than adults.
Mycoplasma pneumoniae
Mycoplasma pneumoniae has been anecdotally observed to be a PANS trigger. The most accurate diagnosis of M. Pneumonia utilizes the information from both polymerase chain reaction (PCR) and serologic testing. IgG titers can be raised for life, even with treatment. Mycoplasma is most often treated with azithromycin, macrolides, and tetracyclines.
Lyme borreliosis
At the time the Treatment Guidelines were published, the PRC did not know of any documented cases in which Lyme borreliosis was a trigger for PANS. OCD and many of the same neuropsychiatric symptoms seen in PANS occur in some Lyme disease patients. Established treatment protocols for Lyme disease should be referenced.
Other infections and triggers
In addition to the infections mentioned above, many other infections are associated with PANS onset and/or exacerbations, including but not limited to varicella, Epstein-Barr virus, enterovirus, dental infection, herpes simplex, gastrointestinal infections. All should be treated as per guidelines for those infections.
For specific more information on Treating PANS PANDAS that is triggered by an infection, please refer to Clinical Management of Pediatric Acute-Onset Neuropsychiatric Syndrome: Part III—Treatment and Prevention of Infections, Michael S. Cooperstock, MD, MPH, et al, Journal of Child and Adolescent Psychopharmacology Volume 27, Number 7, 2017, Mary Ann Liebert, Inc., Pp. 1–4.
We aspire to heal.
Learn about other families whose lives have been affected by PANS/PANDAS — and be inspired to share your own.