PANS & Eating Disorder/Food Restrictions & Toolkits/Handouts
PANS PANDAS & Eating Disorders/Food Restrictions – Full Packet of Recent studies and Flyer. Please note that the Flyer is also available in two poster sizes...
PANS PANDAS & Eating Disorders/Food Restrictions – Full Packet of Recent studies and Flyer. Please note that the Flyer is also available in two poster sizes...

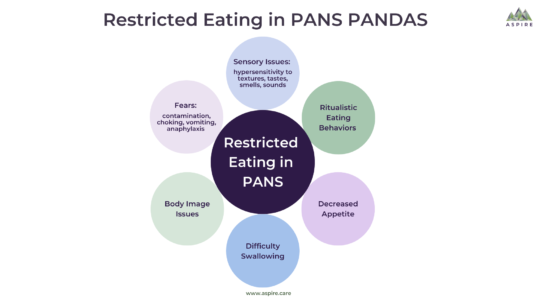
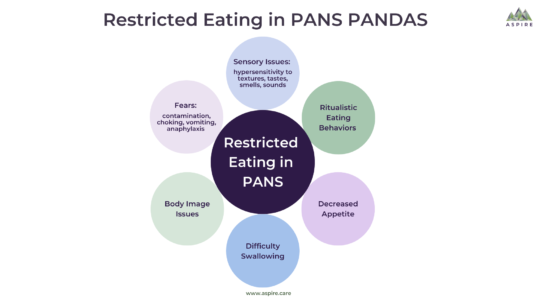
PANS & Eating Restrictions This section on Restrictive Eatings at School is part of a larger section on Restrictive Eating seen in PANS PANDAS. Make sure to read the entire...

Note from ASPIRE: This is a must-read PANS PANDAS Patient Story. A typical happy young girl develops a severe eating disorder and other PANS PANDAS symptoms; then, she suffers through...
Conclusions: The interactions between EDs and autoimmune diseases support the previously reported associations. The bidirectional risk pattern observed in women suggests either a shared mechanism or a third mediating variable contributing to the association of these illnesses.
In a Danish population-based cohort study of 525 643 adolescent girls, a prior infection in childhood was associated with an increased risk of later anorexia nervosa, bulimia nervosa, and eating disorder not otherwise specified.
The findings suggest that hospital-treated infections and less severe infections treated with anti-infective agents are associated with increased risk of subsequent anorexia nervosa, bulimia nervosa, and eating disorders not otherwise specified and that future studies should investigate whether these associations are causal and identify the exact mechanisms between infections and subsequent inflammatory processes with eating disorders.