Neurocognitive and neuropsychiatric symptoms associated with tick-borne disease.
Gabriella: Dr. Roseann, thank you for joining ASPIRE to talk about neurocognitive and neuropsychiatric symptoms associated with tick-borne disease.
Many of our families are dealing with PANS, Lyme, and other tick-borne infections whether or not a tick-borne infection triggered the first PANS symptoms. Some patients’ initial PANS symptoms were triggered by infections like strep, upper respiratory infections, flu, etc. and are also dealing with tick-borne infections while some patient’s symptoms were triggered by tick-borne infections. So no matter which infection triggered initial symptoms or subsequent flares, many patients treating multiple infections at once. Lyme Symptoms
Dr. Roseann: Absolutely. Many patients have both PANS and tick-borne illness diagnosis. It is very taxing on the body to fight so many infections at once, which can make it more difficult to heal. I rarely see someone with just one infection. Once one infection takes hold, and the immune system weakens, then others creep in, which of course, further weakens the immune system. See more about Treatment.
Three Complementary Modes of PANS/PANDAS Intervention
- Remove source of inflammation (infection in this case)
- Treat dysregulated immune system and lower inflammation
- Treat the symptoms.
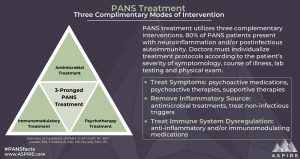
It is a matter of figuring out which infection to treat and how, while addressing the inflammation and the dysregulated immune system and getting the nervous system to calm down so their body can do what it is supposed to do… heal itself. When the nervous system is in a sympathetic dominant state, it is in a constant rev state; it is agitated and not able to appropriately address viruses and bacteria or any infection that is in the body. However, when we calm the CNS and get it to regulate and go into a sympathetic dominant state, it can turn its attention to infection and repair.
Unfortunately, I see patients whose neurological symptoms are misdiagnosed and, therefore, not treated correctly. Lyme and tick-borne disease are complex diseases that produce physical, cognitive, and psychiatric symptoms that present differently in each patient. One person may experience severe joint pain, and another may have brain fog and anxiety. Yet, they both have a tick-borne illness.
Gabriella: What are the neurological symptoms of tick-borne diseases and which ones overlap with PANS Symptoms?
Dr. Roseann: Actually, all. For some kids, they had no pre-existing issues, but with 50 % of American children have a mental health or a physical issue, many children had some kind of challenge. These pre-existing issues and a tendency for some to have some soft signs appear first (constipation, slowed processing, minor sleep issues), makes diagnosing a challenge. And when PANS shows up in a young child, people may mistake it as typical toddler tantrums or just food resistance.
With PANS, there is a sudden onset or an acceleration of symptoms that were already there. For example, your child may have had focus issues but all of a sudden, they literally can’t focus at all. And depending on what issues the child previously had, and when they appear, they really can be hard to tease out. With the Lyme Disease symptoms and, more specifically, the neuro-cognitive symptoms, they typically progress over time and don’t have a sudden onset. In some circumstances, they can.
Gabriella: What are neurocognitive symptoms of a tick-borne disease?
Dr. Roseann:
Neurocognitive Tick-Borne Disease Symptoms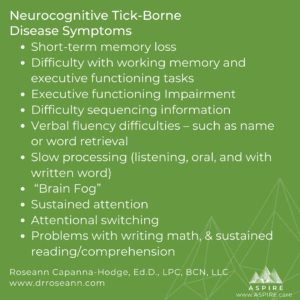
- Short-term memory loss
- Difficulty with working memory and executive functioning tasks
- Executive functioning Impairment
- Difficulty sequencing information
- Verbal fluency difficulties – such as name or word retrieval
- Slow processing (listening, oral, and with written word)
- “Brain Fog”
- Sustained attention
- Attentional switching
- Problems with writing, math, and sustained reading/comprehension
Gabriella: What are neuropsychiatric symptoms of a tick-borne disease?
Dr. Roseann:
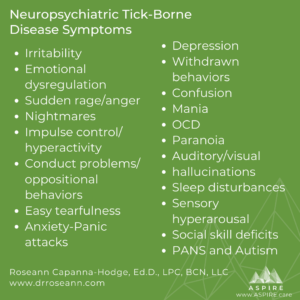 Neuropsychiatric Tick-Borne Disease Symptoms
Neuropsychiatric Tick-Borne Disease Symptoms
- Irritability
- Emotional dysregulation
- Sudden rage/anger
- Nightmares
- Impulse control/hyperactivity
- Conduct problems/oppositional behaviors
- Easy tearfulness
- Anxiety or Panic attacks
- Depression
- Withdrawn behaviors
- Confusion
- Mania
- Obsessive Compulsive Disorder
- Paranoia
- Auditory/visual hallucinations
- Sleep disturbances (too much or too little)
- Sensory hyperarousal (typically auditory, visual, and touch)
- Social skill deficits
- PANS and Autism (it is estimated that 25% of those with Autism have PANS/PANDAS – O’Hara, N. (2014). Lyme Connection Mental Health Conference.
Gabriella: I know this question opens a bigger discussion but briefly, how do the neurocognitive and neuropsychiatric symptoms affect children in school?
Dr. Roseann: These symptoms can have a devastating effect on children’s learning, memory, and overall processing. They may have been a good student and then essentially they can’t think anymore. Their processing is so labored that by the time they figure out what a teacher just said, the class has moved on. For other children, they can have good and bad days and some can even largely “hold it together” during the day except for when they have flares. And these children often have sensory sensitivities to light and sound that make getting through a school day even harder.
Gabriella: Do you have key parenting strategies for handling these symptoms?
Dr. Roseann: Let’s face it; managing the behavioral, emotional, and cognitive issues that come along with PANS and Lyme is rough. Traditional parenting techniques typically don’t work. Nothing about a child with PANS behavior is intentional! But the ups and downs due to a flare can cause a parent to question that. The best way to approach PANS parenting is to set loving limits. Loving limits are clear limits with a flexibility that accommodates for emotional or behavioral distress. It is also important to use positive communication, model emotional language, and to make sure you are using self-care techniques.
Gabriella: What are some of the non-medical treatments you recommend for treating/addressing these symptoms?
Dr. Roseann: It is so important to get that nervous system to calm down, so the body can use its energy to repair and heal.; there are wonderful proven and natural ways to do that. For many years, I have used neurofeedback, biofeedback, PEMF, and very specific types of psychotherapy (ERP for OCD, trauma therapy, etc.) to treat the behavioral, emotional, and cognitive symptoms of PANS and Lyme. These tools pull kids out of the fight, flight, or freeze mode so they can begin to relearn how to apply those brakes and switch gears when paired with psychotherapy. The experience of PANS is so traumatic for both parent and child. I often recommend using trauma therapy techniques such as Somatic Experiencing Therapy and EFT/Tapping to help children and moms to deal with all their pain.
Roseann Capanna-Hodge, Ed.D., LPC, BCN, LLC Integrative and Pediatric Mental Health Expert
Website
Dr. Roseann is a Psychologist, Pediatric Mental Health Expert and the founder and director of The Global Institute of Children’s Mental Health and Dr. Roseann and Associates, a Connecticut-based center that’s helped thousands of children and adults reverse the most challenging conditions such as ADHD, Autism, anxiety, depression, concussion, learning disability, Lyme Disease, and PANS/PANDAS. Dr. Roseann treats these conditions using proven holistic therapies such as neurofeedback, biofeedback, psychotherapy, and nutrition using her trademarked intensive two-week intensive 360 Reboot™ Program. She is the co-author of the best selling book “Brain Under Attack: A Resource For Parents and Caregivers of Children With PANS, PANDAS, and Autoimmune Encephalopathy.” She has been featured on national outlets such as The Mel Robbins Show, Fox News, CBS, NBC, PIX11 NYC, Cheddar TV, Voice of America- VOA, FORBES, PARENTS, Insider, WebMD, and The New York Times.
For more on Lyme Symptoms:
