Lyme disease, PANS, and the Columbia University Lyme & Tick-borne Research Center.
Shannon L. Delaney, MD, Director, Child and Adolescent Evaluation, Lyme & Tick-borne Research Center, is a neuropsychiatrist at Columbia University Irving Medical Center who is co-investigator with Brian Fallon, MD on studies of adults and children with Lyme disease. Her clinical research has focused on immune and infectious contributions to psychiatric disease, especially psychosis in children and young adults. She specializes in seeing children and adults with complex neuropsychiatric presentations, especially those with suspected Lyme disease or other tick-borne illnesses, as well as those with Pediatric Acute-onset Neuropsychiatric Syndrome (PANS). Dr. Delaney provides assessments and a detailed referral with treatment recommendations for children and young adults with complex neuropsychiatric presentations due to a variety of infectious and immune causes of neuropsychiatric disorders. Dr. Delaney’s profile
Gabriella: First, I would like to thank Dr. Delaney for being a member of the ASPIRE Professional Advisory Board. Thank you for taking the time to sit with us and talk about Lyme disease, PANS, and the Columbia University Lyme & Tick-borne Research Center.
Dr. Delaney: Tick-borne illness is so controversial. There is such a spectrum of understanding and treatment that often people encounter doctors who will put them on antibiotics for years and years while other doctors dismiss them and their lab work. There is a huge need for a little more objectivity in the matter. At Columbia, we see people for consultations, not treatment.
Gabriella: So, who is treating your patients that you consult with?
Dr. Delaney: I give them a final medical report. It has all of my thoughts and impressions, along with supporting literature. I usually talk to their primary care doctor. Pediatricians usually follow short-term recommendations. If they don’t, I will refer to another doctor.
Gabriella: When a patient comes to you because they are highly suspecting Lyme disease, whether they have PANS symptoms as well or not, what is the criteria you are using to diagnose them with Lyme disease?
Dr. Delaney: Honestly, that is a tough question as it is truly a clinical diagnosis. So, when people come to see us, I get an extensive history, including the clinical, medical, and psychiatric history. Then we send blood to three different labs.
Gabriella: Let’s talk about testing. What labs are you currently using for Lyme and co-infections?
Dr. Delaney: For Lyme disease, we send testing to three specialty labs. We have traditionally used a western blot through Stony Brook University, Medical Diagnostics Labs, a specialty lab out of New Jersey, and we were using Imugen but Quest just bought them out. They were the only laboratory doing antibody testing for Borrelia miyamotoi except for Igenix. Borrelia miyamotoi is one of the tick-borne infections that causes Tick-borne relapsing fever (TBRF). Symptoms are recurring bouts of fever, headache, muscle and joint aches, and nausea. Co-infection testing we still do through Quest as they are accurate for those infections. We see a lot of variability for Lyme disease, which is why we send out to three labs.
We see a lot of discrepancies in the Western Blot labs. So certainly on the Western Blot, looking at the IgG bands, if we see five bands, it is essentially a definitive diagnosis as per the CDC’s diagnostic criteria. In my opinion, four positive bands are enough. There can be a valid basis for a diagnosis for those with three bands in combination with a convincing history, medical, clinical, and psychological. You cannot make a strong argument for diagnosis in cases with no bands or only one band with no clear clinical history. But if you live in a highly endemic area with some symptoms, then the case can be built.
Gabriella: Can a treatment trial be used to form a clinical diagnosis?
Dr. Delaney: Yes, it can be a variable in making a diagnosis given that is a clinical diagnosis.
Gabriella: Do you see patients who live on the East coast positive for Babesia Duncani? Do those patients have a PANS diagnosis.
Dr. Delaney: Yes, I see patients with Babesia Duncani even though CDC considers it to be isolated to the West coast. The caveat is that the CDC says in order to constitute exposure to Babesia Duncani, you have to have an IgG titer of greater than or equal to (≥) 1:512. The lab we use to test for Babesia Duncani is a public health lab in Sonoma, CA. They report if your titer is reactive at a lower amount, at (≥) 1:256. Most of the kids I see that have a history of Lyme, PANS, and Babesia Duncani, have been positive at that 1:256 level. However, many Infectious Disease doctors believe you must have a positive PCR test to be truly positive. We see patients with clinical signs and symptoms of Babesia, bad nausea, GI symptoms, and abominable pain, which we do not see with Lyme disease very often. So I don’t know exactly what to make of this, but I do think that there are more cases of Babesia duncani than what the infectious disease community thinks based on only positive PCR testing.
Gabriella: What are your current research projects?
Dr. Delaney: We have been working on the protocol for a PANS and Lyme study for the past year. The focus is recruiting kids who have had a probable history of Lyme disease with also PANS type symptoms to understand more about the phenomenology of the disease and collect blood so we can hopefully identify biomarkers. Also, we will be doing neurocognitive testing. Everything is basically approved, but we are delayed due to COVID-19 physically distancing measures.
During this time of precision medicine, our goal at Columbia is to identify essential biomarkers that will guide treatment by indicating who would benefit from additional antibiotic therapy or another approach.
Gabriella: So once you are back, will be taking research participants from your current pool of patients or will you be actively recruiting new participants?
Dr. Delaney: New recruits
Gabriella: When you do start, ASPIRE will share the announcement and link to the study and its requirements. We have a section on the ASPIRe website on current studies being recruited for.
Dr. Delaney: We will definitely share the study information for ASPIRE to share. That would be fantastic.
Gabriella: Any other studies?
Dr. Delaney: We are doing a study with adult patients using Disulfiram.
Gabriella: In your patients, has Lyme been the initial trigger of PANS symptoms or do find that the neurocognitive symptoms of Lyme that are PANS symptoms as well have come on gradually, so they are two co-occurring conditions?
Dr. Delaney: A child with acute onset of neuropsychiatric symptoms, such as obsessive-compulsive disorder, restricted eating, sensory issues, urinary frequency, anxiety, cognitive dysfunction, or extreme fatigue, should be given a set of lab tests to rule out typical infectious causes of PANS/PANDAS.
I am not really seeing these patients in the acute phases, so it is hard for me to always tell what was happening when. I do speak with many pediatricians while their patients are in the acute phase, and so I do see patients in which Lyme disease has 100% triggered the acute-onset of PANS symptoms. Then when they come to see me, I do see the abrupt onset due to Lyme disease in their history. I also have many patients with a history of Lyme disease and other tick-borne illnesses who do not present with PANS symptoms. Many do have neurocognitive symptoms but not the cluster of symptoms described by the PANS diagnostic criteria as they don’t have the behavioral dysregulation and those more typical of PANS.
Gabriella: Do those Lyme and co-infection patients without PANS who still have neurocognitive symptoms have separation anxiety seen in most patients with PANS?
Dr. Delaney: No, not usually. There is a certain amount of them that have more of the main physical symptoms. They don’t have the neuropsychiatric issues as much.
Gabriella: Do they have the brain fog and the slower processing skills?
Dr. Delaney: It is a little harder to articulate in the younger kids. I see a ton of teenagers who don’t have the PANS symptoms but do have the neurocognitive brain fog and difficulties at school, along with being physically ill with a lot of significant fatigue. It is very common for the kids to go on medical leave from school.
Gabriella: Is there additional testing you order, aside from the bloodwork?
Dr. Delaney: As you know, these kids have immensely complicated histories. If a patient presents with a history and labs that is not clear cut Lyme or tick-borne disease, I sometimes will order a spinal tap. Spinal taps are usually not that helpful for PANS and Lyme. If I am suspicious that there is another neurological condition that might be contributing, I sometimes lean towards a spinal tap. It gives us more generalized information. If there are more neurological impairments, that is when I push for one.
Gabriella: What treatments do you recommend in your reports? You see complicated cases and treatment recommendations are individualized, but is there some semblance of a set protocol?
Dr. Delaney: Not really. But Doxycycline, Amoxicillin, and Ceftin are the first-line treatments for Lyme disease. If the kid is not really young, I typically recommend Doxycycline because it has pretty good penetration of the blood-brain barrier; it gets into the brain pretty well. If they are younger, I usually say Amoxicillin.
Azithromycin is not a first-line treatment for Lyme disease. I do recommend Azithromycin if the patient presents with a history of Lyme with PANS type symptoms and are positive for Babesia Duncani. The treatment for Babesia Duncani is usually Azithromycin and Mepron together.
So, typically I recommend to PANS patients with a history of Lyme, a month-long course of Doxycycline. If that works, I then sometimes recommend Azithromycin as that works for so many patients with PANS. It can be helpful in treating Lyme disease, although it is not a first-line treatment for Lyme.
Gabriella: What are your thoughts on the use of IVIG in Lyme PANS patients?
Dr. Delaney: We see adults and kids with a history of Lyme disease, even without PANS, who benefit from IVIG. Depending on the situation, sometimes I run an autoimmune neurology panel and often check for thyroid antibodies. If any of the autoimmune antibody workup is positive, and they have had antibiotic treatment while they still have ongoing symptoms, that is when I bring up that they should consider IVIG. So those things together: chronic symptoms, adequate antibiotics, plus evidence of a continued autoimmune component to the disease is when I think it is time to consider IVIG.
I see many kids and adults who will be positive for thyroid antibodies and have a history of tick-borne illness. Actually, I see this way more than what I would expect, so it is certainly perplexing.
Gabriella: Do you recommend Plasmaheresis?
Dr. Delaney: To my knowledge, that doesn’t have as much literature backing it up. I don’t see a lot of the Lyme specialists using it as much.
Gabriella: What about steroids to tamp down the brain inflammation when Lyme is in the mix?
Dr. Delaney: I don’t really ever recommend steroids. They can suppress the immune system. It is not recommended in the setting of Lyme disease. I don’t see patients who have PANS with Lyme or just Lyme improve from steroids. I see the neuropsychiatric symptoms getting a lot worse more often than making them better.
Gabriella: What other diagnoses do you see Lyme treatment helping?
Dr. Delaney: Certainly, the most common diagnoses we see are Anxiety and Depression. Pretty much everyone we see with chronic symptoms of Lyme disease, by the time they get to us, usually have anxiety, depression, or both.
Gabriella: Do you have an idea about what is causing that? Inflammation? The fact that it is hard to be sick that long and how frustrating it is to live with chronic illness?
Dr. Delaney: I wish I had the answer there. Some of them have a history of anxiety or depression predating when they first got Lyme disease, but some don’t have any history of it. My best guess would be that it is a mix of the inflammatory theory that the inflammatory molecules are contributing. Probably just as important is that these patients are often very disenfranchised from the medical community. The doctors often don’t understand about tick-borne illness. Some tell patients that they don’t have a diagnosis of Lyme disease. That can lead to them not having family support since the families agree with the doctor. Not having a correct diagnosis and not being validated by the medical community is a huge contributor to anxiety and depression.
Gabriella: We do know with PANS that the rate of depression increases in the older patients and the patients that have had multiple relapses and are not getting better. This is no surprise because it is hard to be chronically ill and live in fear of when the next relapse will happen and whether you will get better in addition to years of brain inflammation. Constant Stress Disorder, we never get a chance to even experience PTSD since we are not in the “Post” position.
Dr. Delaney: Totally agree. I have a few teenage patients with a history of PANS when they were in elementary school. I was not their doctor back then. But they recovered from the PANS and its symptoms but now are dealing with Lyme or other tick-borne illness and now have depression.
Gabriella What about bipolar and Lyme? Do you see an overlap?
Dr. Delaney: In my research study, during my fellowship, I recruited patients with psychosis and found a surprisingly high number of participants with a history of Lyme disease. However, this was complicated because there was some referral bias from the Lyme center and the fact that in most situations, the history of Lyme disease and the symptoms of psychosis were not proximally related. There are some case reports showing symptoms of psychosis emerging in the context of neurological Lyme disease and improving with antibiotics. This remains an area of interest to me, and I think it needs to be explored more.
Gabriella: The CDC says that 300,000 Lyme disease cases are reported each year, and the number of cases is increasing in both incidences and distribution. Plus, we know that many cases are not reported because of the lack of truly reliable testing. Can you talk a bit about that?
Dr. Delaney: NY and surrounding areas have such high rates of Lyme and tick-borne illness throughout the year that we cannot underestimate how often people are exposed and contracting these diseases. So, even if Lyme testing is not always so clear-cut, we must carefully consider that clinical picture with the mindset that we are in a highly endemic area. Rafal Tokarz from the Center for Infection and Immunity at Columbia University was part of the team that published a study on the Polymicrobial Nature of Tick-Borne Diseases. The study showed, 57% of the adult and 27% of nymphs Ixodes scapularis ticks, deer tick or black-legged tick, the ones that carry Lyme disease, were positive for Lyme disease.
Gabriella: Further driving home that we need to be vigilant about tick control and prevention the entire year.
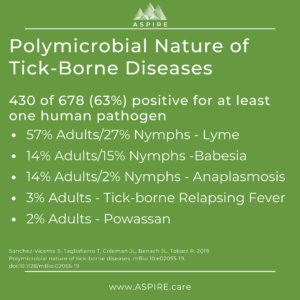 Dr. Delaney: Yes, absolutely. This same study showed that polymicrobial infections were detected in 22% of the ticks and 63% test positive for at least one pathogen. So the point is if you are living in a Lyme endemic area and you are having symptoms that could be suggestive of Lyme disease, noting that sometimes Lyme can present very strangely with neurologic symptoms only or even vague symptoms, it is probably beneficial to look into at least short-term treatment, even if you don’t have confirmed laboratory diagnosis.
Dr. Delaney: Yes, absolutely. This same study showed that polymicrobial infections were detected in 22% of the ticks and 63% test positive for at least one pathogen. So the point is if you are living in a Lyme endemic area and you are having symptoms that could be suggestive of Lyme disease, noting that sometimes Lyme can present very strangely with neurologic symptoms only or even vague symptoms, it is probably beneficial to look into at least short-term treatment, even if you don’t have confirmed laboratory diagnosis.
Gabriella: There we go. I am glad you said that. Many people need to read that and know this. Those numbers are really frightening.
Dr. Delaney: Agree, it is shocking.
Gabriella: Thank you so much. That was certainly informative. I know everyone will love learning more about the Lyme & Tick-borne Research Center at Columbia and their approach. Any closing thoughts
Dr. Delaney: Physicians need to have heightened awareness of Lyme disease and PANS/PANDAS. They must also have a clinical suspicion of Lyme in children who present with neuropsychiatric symptoms. Lyme disease must be diagnosed promptly, and patients need to be provided with appropriate treatment, which may include referral for appropriate symptom management.
