 ASPIRE thanks the NECH team for continuing to host talks and having ASPIRE write notes to share with the community. Patients of Dr. O’Hara and Dr. Wells can ask additional questions in the patient portal. Please check back for the upcoming schedule as well as Q&As and transcripts of previous meetings. NECH Educational Sessions. Patients with additional questions can message Dr. Wells, Vicki Kobliner, and Dr. O’Hara in the portal.
ASPIRE thanks the NECH team for continuing to host talks and having ASPIRE write notes to share with the community. Patients of Dr. O’Hara and Dr. Wells can ask additional questions in the patient portal. Please check back for the upcoming schedule as well as Q&As and transcripts of previous meetings. NECH Educational Sessions. Patients with additional questions can message Dr. Wells, Vicki Kobliner, and Dr. O’Hara in the portal.
Multi-System Inflammatory Syndrome with COVID with Nancy O’Hara, MD and Lindsey Wells, ND
Multisystem Inflammatory Syndrome (MIS-C)
- Recognized on April 26, 2020 by UK clinicians
- Previously healthy children present with severe inflammatory syndrome with Kawaski Disease like features
- These children tested positive for or had exposure to COVID-19
Some people have called MISC-C, the Kawasaki like syndrome, the multi-system inflammatory syndrome, or the toxic shock syndrome. It really is a multi-system inflammatory syndrome that is associated with COVID-19 in children. This was first recognized by clinicians in the United Kingdom as well as others in Italy, and then in the United States. We are seeing previously healthy children presenting with an inflammatory disease that looks a lot like Kawasaki disease. Kawasaki is an illness that causes the blood vessels to become inflamed. It’s almost always in young children, and this particular disease has a slightly older profile. It is a leading cause of heart disease in children, and that’s one of the things we want to look out for and to treat.
Symptoms
- Kawasaki disease causes blood vessels to become inflamed, almost always in young children. It’s one of the leading causes of heart disease in kids. But doctors can treat it if they find it early.
- Signs of the first phase of Kawasaki disease include:
- High fever (above 101 F) that lasts more than 5 days. It won’t go down even if a child takes medication that usually works on fever.
- Rash and/or peeling skin, often between the chest and legs and in the genital or groin area
- Swelling and redness in hands and bottoms of feet
- Red eyes
- Swollen glands, especially in the neck
- Irritated throat, mouth, and lips
- Swollen, bright red “strawberry tongue”
- In the second phase, symptoms include:
- Joint pain
- Belly pain
- Stomach trouble, such as diarrhea and vomiting
- Peeling skin on hands and feet
- Kawasaki disease can cause heart trouble 10 days to 2 weeks after symptoms start.
The symptoms we see are a conjunctivitis type of symptom with red eyes, also inflamed red cheeks, swollen red hands with peeling fingers, or swollen red feet. Probably one of the precursors of this, which we saw many weeks ago, was COVID toes, which is swelling and redness of the toes and purpura, which is a breakdown of the blood vessels or petechiae, a breakdown of the tiny blood vessels called capillaries. Red cracked lips and tongue, high fever and a rash covering much of the body. It can present with peeling skin. The rash can be in the genitalia or the groin area, or on the chest and legs. You may see swollen glands, especially in the neck, and maybe joint pain, belly pain, diarrhea, and vomiting. These children that were tested in the UK and in Italy tested positive for coronavirus with either an IgG or IgM test.
Literature Review
Hyperinflammatory Shock in Children During COVID-19
- The Lancet article reported on a period of 10 days in April when there was a cluster of eight children in the UK that presented with a hyperinflammatory shock similar to atypical Kawaski Disease
- Clinical presentation included fever, variable rash, conjunctivitis, peripheral edema, generalized extremity pain, GI symptoms.
- Most children had no significant respiratory symptoms.
- Seven required mechanical ventilation for cardiovascular stabilization. One died.
- All were either PCR- or antibody-positive for SARS-CoV-2. That’s important—it seems like this syndrome can occur in the convalescent phase of the illness.
This study reported on these children with MISC-C and COVID in the UK. This article looked at children over a period of 10 days, during which there was a cluster of 8 children presenting with this hyperinflammatory shock illness similar to Kawasaki disease. They noticed there was fever, a variable rash, conjunctivitis, some edema in the extremities, and some pain in the extremities and some GI symptoms. What was interesting about this is the children did not have significant respiratory symptoms, like we’ve seen with COVID-19 across the board.
These children, seven out of the eight of them, did require some mechanical ventilation for cardiovascular stimulation and stabilization. Unfortunately, one of them passed away. All of the children were either PCR or antibody positive for COVID-19. It’s important to know that it was also found in children outside of the acute phase of COVID-19; they saw it also in the convalescent phase after an active infection.
Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395(10237):1607‐1608. doi:10.1016/S0140-6736(20)31094-1
An Outbreak of Severe Kawasaki-like Disease at the Italian Epicentre of the SARS-CoV-2 Epidemic: An Observational Cohort Study
This is Lancet article reports on the Kawasaki like disease in Italy in the Bergamo province, which was the hardest hit area of Italy. They compared their typical cohorts of the last several years with a cohort between February and April of this year. They compared 19 patients who had this syndrome between January 2015 to February 2020, with 10 patients from February 2020 to April 2028, 8 out of 10 had positive IgM or IgG antibody tests to COVID-19.
The patients between 2015 and 2020 had a median age of three. The patient’s with COVID-19 had a median age of seven and a half. There’s also increased cardiac involvement, increased shock, or hypotension, meaning low blood pressure, increased macrophage activation, meaning that they have low platelets, low white blood cells, and an increased need for steroids. The group was mostly male. In the classic Kawasaki cases from 2015 to 2020, 19 had the very classic Kawasaki symptoms. In the COVID group, 5 out of 10 had classic symptoms. Also, in the COVID Group, the sed rate was markedly elevated, and all of them, five of them had pneumonia. Six had an abnormal echocardiogram or ultrasound of their heart, and six had diarrhea.
The other interesting section in this article was they mentioned a coronavirus outbreak, a different coronavirus; the cold is a coronavirus, in New Haven in 2005. Eight of eleven children with Kawasaki disease diagnosed in that year tested positive for coronavirus. So the point is that this particular virus is known to be a trigger for a Kawasaki-like disease.
The last point from this article is that 19 patients from 2015 to February 2020 versus 10, from February to April 202, there was a 30 fold increase in seeing this type of disease.
Verdoni, Lucio et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet, May 13, 2020. DOI:https://doi.org/10.1016/S0140-6736(20)31103-X
COVID-19 in Kids: Severe Disease Most Common in Infants, Teens,
- This reported on 177 infected children in the DC area. 44 required hospitalization. 9 were critically ill.
- Children under 1 years old and adolescents/young adults >15 years old were over-represented in the hospitalized patients
- Adolescents/young adults were over-represented among the critically ill cohort
- Underlying medical conditions present in 39% of all patients with COVID 19 infection. The most frequent underlying diagnosis: asthma, neurological, diabetes, obesity, cardiac, hematologic, oncologic
- Underlying conditions were more common as a whole in the infected hospitalized cohort compared to the infected non-hospitalized cohort
- Although asthma was the most prevalent underlying condition, it was not more common in the hospitalized cohort. Asthma is not the primary determinant of more severe disease requiring hospitalization.
- 8 of the 9 critically ill patients required respiratory support (mechanical ventilation). 1 of 9 presented with the Kawaski-like disease presentation
This article looked at children in the DC area. This was a group of 177 infected children in the DC area. Out of those 177 children, 44 required hospitalization, and then 9 were considered critically ill. There were two cohorts. There were children under a year old year that had an increase in hospitalizations. There were also adolescents and young adults over the age of 15; this group had the majority of the hospitalizations. The adolescents and the young adults were over-represented in that critically ill category. Nine of the 177 were critically ill; all of them were above the age of 15. 39% of all the patients had underlying medical conditions. The underlying issues include asthma, obesity, diabetes, some neurological disorders, some cardiovascular, and cancer. They found that hospitalized patients had more underlying medical conditions than non-hospitalized patients.
Although asthma was the most prevalent underlying condition, it was not more common in the hospitalized cohort, which means that asthma is not a primary determinant of a more severe disease that requires hospitalization. Also, in the critically ill cohort, eight out of the nine patients required some respiratory support—only one out of the nine presented with the Kawasaki like disease presentation. Although there has been a significant 30% increase, it’s still rare. To recap, out of 170 children, 9 were critically ill and 1 presented with a typical presentation of Kawasaki.
COVID-19 in Kids: Severe Disease Most Common in Infants, Teens, Heidi Splete, Med Scape – May 19, 2020
MIS-C Associated with COVID19 New York City Department of Health and Mental Hygiene Report
New York State Department of Health
- As of May 13, investigating 110 cases of MIS and three deaths
- The age distribution suggests the highest risk is in the 5-14-year range
- Older kids with the syndrome may be diagnosed simply with COVID-19, which can lead to severe illness.
- In New York, just 1% of those hospitalized are under the age of 20, which is around 750 kids. With 110 cases, MIS is not super rare, at least among those kids who are sick enough to get to the hospital.
- If 100,000 kids were infected with COVID-19, we’d expect 5000 to be hospitalized. We’d expect 733 cases of MIS. Of those, we might see 20 deaths = 0.02%
- The racial breakdown in New York City seems to be consistent with population averages
This report looked at the disease in New York. And as of May 12th, 2020, there were 102 patients that were identified with this MIS-C. From April 16 to May 4, 15 patients were hospitalized, some to the intensive care unit. They were between the ages of 2-15. So not the young adults that we’re seeing in some of the other studies but certainly a higher age group than previously considered for Kawasaki. The 5 to the 14-age range has the majority of the cases.
Also, in New York, the kids with MIS-C follow the typical population averages. What we see is a typical pattern of African Americans, Caucasian, and Asian populations as compared to the racial breakdown of deaths in New York overall, not just children. The death rate is very disproportionate among the African Americans population at 41% compared to the Caucasian population at 12%, Latino at 29%, and Asian at 18%. So, MIS-C is not following the same pattern of racial discrepancies seen with typical COVID-19 symptoms.
Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19). CDC Health Alert Network May 14, 2020
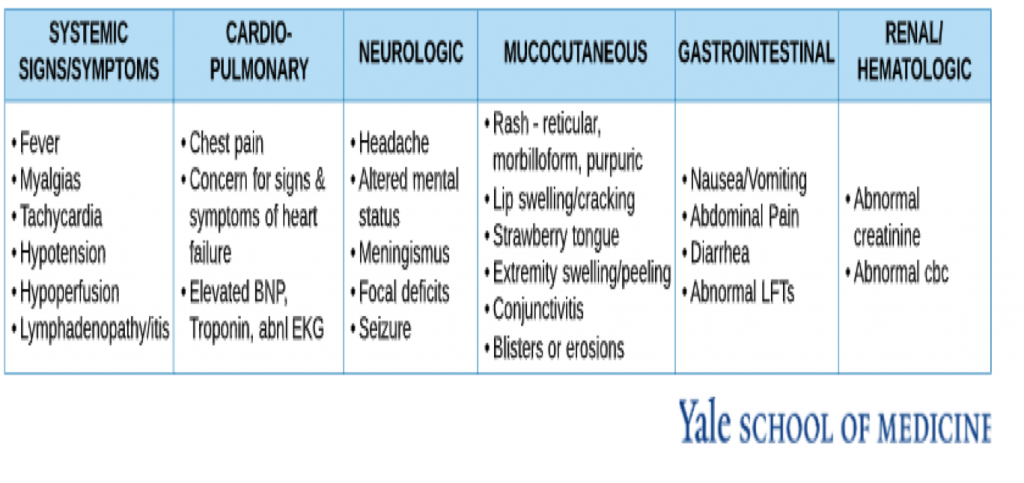
Symptoms
- Persistent fever (>100.4)
- Hypotension
- Multisystem (>2) organ dysfunction
- Cardiac
- Renal
- Respiratory
- Hematological
- Gastrointestinal
- Dermatological
- Neurological
If you see these symptoms, we really feel you should contact your primary caregiver. This includes persistent fever, a fever longer than 5 days, and anything over 100.4 degrees. Hypotension can be seen in a child who passes out, feels very weak, or may have blueness in the tips of their fingers or their toes. They may feel very thirsty.
The third category is when more than two organs are affected. Systemic signs and symptoms include fever, muscle aches, tachycardia (heart beats faster), low blood pressure, hyperperfusion, and sometimes swollen glands. Cardio-pulmonary symptoms include chest pain, signs and symptoms of heart failure – hypotension, low blood pressure, hypoperfusion, and passing out. Then the others are things that are found when the child gets checked by the doctor – abnormal EKG or elevations of cardiac markers. Neurologic symptoms include headache, acting confused, or lethargic. They may have signs of meningitis, which can be seen when you try to push their chin down to their chest, and they resist because it’s painful. There are certainly more severe focal deficits, as you would see in a stroke or seizure. Skin symptoms include rashes of any kind all over the place. Rashes can be purpuric (looks like a purple bruise). It can be morbilliform or reticular (lacy). There can also be lips swelling, cracking, or a strawberry tongue. The can be peeling of the fingers and toes. Conjunctivitis, blisters, or erosions anywhere can be seen. Gastrointestinal issues include nausea, vomiting, diarrhea, etc. Renal and Hematologic signs present as kidney disease, or there can be low white blood cell counts and low platelet counts.
The Disease is Rare
Remember, MIS-C is rare. We are discussing it, so you know what to watch out for, but it is still very rare. There are thousands and thousands and thousands of cases COVID. There are only cases of MIS-C in the low hundreds in New York, which is one of the hardest hit areas. So far, there are probably a dozen cases in Connecticut.
Laboratory Evidence
- PCR positive for COVID 19 OR COVID 19 exposure within 4 weeks of onset of symptoms
- Additional laboratory evidence:
- Elevated inflammatory markers
- CRP, ESR, Procalcitonin, D-dimer, Ferritin, Neutrophils, Fibrinogen, LDH and/or IL-6
- Decreased lymphocytes and/or albumin
- Elevated inflammatory markers
Lab evidence of the multi inflammatory syndrome is a PCR positive for COVID-19 or exposure within four weeks of symptom onset. Additional laboratory evidence can be done with additional blood work. This includes elevated inflammatory markers such as C-Reactive Protein (CR), Sed Rate (ESR), Procalcitonin, D-dimer, Ferritin, Neutrophils, Fibrinogen, LDH, and/or IL-6. Il-6 is a pro-inflammatory cytokine. Also, what can be seen is that there are some decreased lymphocytes and or albumin. Again, that ‘s expected when there is an infection and, therefore a lot of inflammation.
Treatment
- Steroids
- Anticoagulation
- IVIG
- Antibiotics
- Other immunomodulators
These medications are for the treatment of MIS-C, not for prevention. The treatments that are being used are steroids, anticoagulants, IVIG, antibiotics, particularly in those with meningitis or pneumonia with the chance that this is secondarily bacterial, and other immune modulators like plasma and rituximab. So the typical course of treatment for hospitalized patients or those that are being treated for MIS-C is steroids and then moving on to IVIG and sometimes antibiotics.
If You Think Your Child Has MIS-C
Contact your child’s pediatrician right away if experiencing the following symptoms:
- Fever
- Abdominal pain
- Vomiting
- Diarrhea
- Neck pain
- Rash
- Bloodshot eyes
- Feeling extra tired
** Note: Not all children will have all the same symptoms
Seek emergency care – 911 – right away if your child is showing any of these emergency warning signs of MIS-C or other concerning signs:
- Trouble breathing
- Pain or pressure in the chest that does not go away
- New confusion
- Inability to wake or stay awake
- Bluish lips or face
- Severe abdominal pain
These are the signs that it really is urgency. This is when you call 911.
Conclusions
- We still don’t know enough about MIS-C
- It is rare (<1%)
- It is important to be aware of symptoms and contact pediatrician
- Continue to focus on supporting your child’s immune system
- diet
- anti-inflammatories
- antioxidants
We still really don’t know enough about this disease. It is very rare. It’s important to be aware of the symptoms and when to contact your pediatrician or the primary care provider. It’s important to continue to focus on supporting your child’s immune system at this time.
Preventative Measures
There are many things that you can do in regards to diet, anti-inflammatories, and antioxidants. These are the things you can do not matter if your child is healthy and neurotypical or if they have autism or PANS/PANDAS.
Diet
- Whole food, organic, and non-processed diet
- Include foods high in antioxidants: Berries, artichokes, kale, spinach, beets, dandelion greens, red cabbage, dark chocolate, etc.
- Culinary herbs and spices: Ginger, Garlic, Cilantro, Parsley, Thyme, Rosemary, Oregano, Turmeric, etc.
- Increasing Vegetables
- Healthy Oils – extra virgin olive oil, coconut oil, avocado oil
- Grass fed organic meats, wild caught fish
- Increasing H2O
- Remove sugars, additives, gluten, casein, soy, sensitivities
Diet is the most important. Food is medicine. So, as much as possible, eat a non-processed, non-refined diet that is organic and filled with whole foods. Antioxidants are all listed; it’s not chocolate; it’s dark chocolate; there is a difference. Use herbs and spices, particularly garlic, ginger oregano, turmeric, adding little sprinkles to anything. Give them potato chips and add sprinkles of this stuff. Healthy oil includes olive, avocado and coconut oil. Meats should be grass-fed organic and wild-caught fish. Drink lots of water. Remove additives, sugars, gluten, casein, soy, and any food sensitivities as much as possible. Basically, this is an anti-inflammatory, healthy diet.
Anti-Inflammatories
- Essential Fatty Acids–Omega 3 (EPA/DHA) & 6 (GLA)
- Eat Sardines!
- Modulation of inflammatory reactions, lowering triglycerides, nerve transmission (Belluzzi et al, 1996)
- Aloe
- Antioxidant properties to decrease ROS (Landmead et al, 2004)
- Curcumin
- Efficacy of curcumin, and a saffron/curcumin combination for the treatment of major depression: A randomized, double-blind, placebo-controlled study (Lopresti et al, 2017)
- Flavonoids – Quercetin, Luteolin, Rutin
- Potent mast cell stabilizer inhibits release of histamine & inflammatory mediators
- Prevents excessive release of histamine(Chuenkityanaon et al, 2010)
- Quercetin is a zinc ionophore and Inhibitor of heat shock proteins needed for viral assembly
- SPM
- Inhibits the NLRP3 inflammasome and decrease IL-1b production found in sepsis and cytokine storm
- CBD Oil
- suppression of cytokines and chemokines at inflammatory sites and upregulation of FoxP3+regulatory T cells (Nagarkatti et al, 2009)
It is important to consider implementing anti-inflammatories. These are some of our favorites to add in. Essential fatty acids, these are your omega-3s – EPA and DHA. The best food source or a very good food source is sardines. It can be hard to get children to eat sardines. Many adults don’t really love sardines. But you can consider supplementing with it. There’s been research showing how it’s able to modulate different inflammatory reactions. It helps to lower triglycerides and can help with nerve transmission. Nerve transmission is how communication is transmitted from one cell to another. It can help with brain health detoxification. Another anti-inflammatory we use often is aloe. It can help reduce the reaction oxygen species that can increase inflammation. We often use that for children who are constipated.
Another one that you can get through a food source or you can get it in higher doses through a supplement is curcumin, also known as turmeric. Tumeric has been shown to help with inflammation. There’s a study that looks at the use of curcumin through mental health perspective and how it can help with depression. We’re seeing that many health issues can be treated with anti-inflammatories because of the association of depression with inflammation.
There are flavonoids you can consider, quercetin, luteolin, and rutin. These are potent mass cell stabilizers. They help stabilize the mast cells that contain histamine in order to prevent histamine release or inflammation or allergies.
Quercetin has also been touted to be helpful with treating COVID-19 because it is a zinc ionophore, which means that it helps to get zinc inside of the cell. Zinc has potent antiviral activity against RNA viruses, which coronavirus is. In addition, quercetin is also an inhibitor of the heat shock proteins that are needed for the viral assembly.
Next is SPM. These are Specialized Pro-resolving Mediators. They have been shown to inhibit the NLRP3 inflammasome and decrease pro-inflammatory cytokine IL-1b, which can contribute to the cytokine storm or sepsis we are seeing in COVID.
The last one is CBD oil or hemp oil. This has been shown to suppress pro-inflammatory cytokines, which increase inflammation in the body. It also helps to increase the fox p3 regulatory T cells. All of these are good options to consider working with your provider to give you the proper dosages that would be beneficial.
Antioxidants
- Vitamin D
- Neuroprotective, immunomodulation, upregulates gamma glutamyl transpeptidase and subsequently increases glutathione (Prufer et al, 2000)
- Vitamin D insufficiency and deficiency correlated with COVID 19 severity and mortality (Raharusuna et al, 2020)
- Vitamin A
- Enhances the immune system, antiviral properties, reduces ROS (Fiedor and Burda, Nutrients, 2014)
- Zinc
- 300 enzymatic functions; in energy metabolism, protein, immunity, detox
- Inhibits replication of RNA type viruses (such as SAR-Cov-2) by blocking RNA dependent RNA polymerase
- Vitamin C
- Antiviral, antibacterial, involved in metabolism of neurotransmitters, iron absorption, collagen production
- Studies report benefit with IV Vitamin C for supportive treatment of COVID-19 (Paul Anderson)
- Resveratrol
- Resveratrol inhibited MERS COV infection and prolonged cellular survival (Lin et al, BMC Infec Dis. 2017)
- Melatonin
- Controls sleeps wake cycle
- Maybe protective in COVID-19 (Zhou et al, Cell Discov. 2020)
- Glutathione
- Master antioxidant
- Case reports of glutathione relieving dyspnea associated with COVID-19 pneumonia (Horowitz et al, Respiratory Med Case Reports, 2020)
Antioxidants are very important. Vitamin D and has been shown, even in allopathic literature, that insufficiency and deficiency are correlated with the severity and mortality with COVID-19. Vitamin D, we know, has many different properties. It is very important for immune modulation, protection of the nervous system, up-regulating gamma glutamyl transpeptidase, and in increasing glutathione in general. Vitamin A is also another enhancer of the immune system; it has been shown in multiple studies to have very important antiviral properties. Zinc is important in greater than 300 enzymatic functions, and it inhibits the replication of RNA Type viruses, which COVID is one of them. Vitamin C is another antiviral; studies have reported in COVID-19 that IV vitamin C is supportive for treatment.
Resveratrol is a potent antioxidant. There was a study done in 2017 that showed that resveratrol could inhibit the MERS COVID infection and prolong cellular survival. MERS is in that family of Coronaviruses. Resveratrol is in Japanese knotweed. So we will use that because it also has antimicrobial benefits. Japanese Knotweed can help against Lyme, Lyme co-infections like Bartonella, as well as yeast overgrowth.
Melatonin is a hormone that is secreted by our pineal gland, and it controls the sleep-wake cycle. It has been suggested, through some research, that it might be protective in regards to COVID-19. They think that might be why children are more protected than adults because they have more melatonin than adults do.
Glutathione is known as our master antioxidant. Case reports published recently show that IV Glutathione, with the addition of it in supplement form helps to relieve the dyspnea caused by the respiratory infections from the COVID-19 pneumonia is very helpful.
Questions Answers
Q: Do these symptoms come in any particular order or all at once?
A: Many come all at once. But again, as we said, you do not have to have all the symptoms. You do not always have to have a rash. You need to have two from the grouping discussed in the symptoms section.
Q: Is there always a rash?
A: No, not necessarily. Rashes seem to be common.
Q: Would kids with Lyme or allergies be at greater risk?
A: So, based on what they were reporting in DC when they looked at that grouping of 177 children, it didn’t seem that Lyme or allergies would put one at greater risk for hospitalization or be critically ill. They did note that there is a possibly greater risk for those underlying conditions like asthma, obesity, or diabetes, possibly that would be increased risk for hospitalization. So, again, there’s still a lot of information that we need to know.
We have to continue to support our immune system, which you are already probably doing if your kid has PANS/PANDAS or Lyme. In our practice, when COVID has been in the family, the children have done very well. Certainly, we worry about our children with autoimmune disease being more at risk. But that’s why we included information on antioxidants, anti-inflammatories, and diet.
Q: What are your thoughts about sending kids to camps or other summer activities?
A: I think we have to make sure that we’re doing things safely. If a hockey team or a soccer team or a camp is doing things safely with as much social isolation as possible, with good handwashing, with wearing masks, then I think it’s definitely worthwhile. If a child is in New York and they’re not planning on wearing masks, they’re using the locker room, and they’re sitting right next to each other, then I’m not sure that I personally would consider this to be safe at this point. It depends very much on where you live and what the recommendations are for your area. Children need to be outside. They need to be in the dirt. They need to play with pets and animals. But they also need to be appropriately socially distance.
Q: Can you have MIS-C with a mild presentation of COVID?
A: So again, there’s still more information that needs to be known about this. With a mild presentation, you can have some of these symptoms, and then you might not seek medical care. The COVID toes, which we have seen in some of our families, are the mildest of mild vascular damage. I think this, like everything else, will run the spectrum. We just are talking about the most severely affected kids because that’s who’s been presented to the hospitals and who’s been studied in the research articles thus far.
Q: Is it possible for COVID to live in the GI system and hide from a positive antibody or active infection test?
A: I think the most important thing is that COVID testing is not 100% accurate. We have found multiple people who fit the profile of having COVID and have negative nasal pharyngeal cultures and also have a negative antibody test. So, yes, you can definitely have COVID and have a negative test. I think it’s a combination of history, physical exam, and testing that needs to be done to say yea or nay whether it is a COVID infection.
Q: What are SPMs?
A: SPM is a specialized pro-resolving mediator. They are potent anti-inflammatories, and you can get it in supplement form. What’s good about them is they are small soft gels, unlike fish oils capsules, which are large. Metagenic has an SPM I’ve used before.
Q: Is multi-system inflammatory syndrome the same as Kawasaki disease?
A: No, but it is very similar. It is a Kawasaki-like disease. It can be different in severity and different in presentation. But if you think your child had it, then it is important to talk to your doctor about it, to look at all the symptoms that were there. If you think they’ve recovered, I would follow up with your primary caregiver because it is important to make sure that there was no cardiac involvement.
2 comments to Multi-System Inflammatory Syndrome with COVID
Riya
August 30, 2020Really good article. Do we know about short term and long term brain effects of MIS-C ( if it co-exists with pandas\lyme or even if it doesn’t) ?. Does it lead to irreversible brain damage ?
FLORIE GLUSMAN
September 8, 2020my incredibly healthy 15 year old daughter is presenting with severe tics…. we are assuming pans related….. i had a moderate covid case in march but she, her siblings and dad were asymptomatic just fatigue and headaches…… wondering if you are seeing any severe tics/pans like symptoms from this…..