PANS PANDAS & Food Restriction/Avoidance
If your child has new or suddenly increased food avoidance or eating restriction along with other behavior, neurological or cognitive changes, it might be due to PANS/PANDAS. Food restrictions and OCD are the two top-tier symptoms of PANS. For more information on PANS PANDAS Symptoms

Click the button below to download the twelve-page toolkit that provides information on Restricted Eating in PANS PANDAS.
Register with ASPIRE to download this information toolkit.
PANS & Restricted Eating Toolkit
ASPIRE has two additional PANS & Restricted Eating Handouts. One is a general information handout that can also be downloaded as a poster. The second handout is Restrictive Eating in School. Please see the end of this article to download those.
Additional ASPIRE Resources
Main Article Sections
- PANS & Restricted Eating
- Treatment for Restricted Eating Due to PANS
- Restrictive Eating at School
- Relevant Studies
- Other Eating Disorders
- Other Resources
- Other Handouts
PANS & Restricted Eating
Restricted Eating and OCD are the two major symptoms in the diagnostic criteria for PANS. Roughly 50% of PANS patients will have some degree of restrictive eating, and about 17% will have life-threatening issues as a result. Restrictive eating can include both food and fluids. Restrictive eating includes avoidance of particular foods and fluids and restricting the intake amount.
People with PANS restrict eating due to disordered sensory hypersensitivity, obsessional fears, difficulty swallowing, decreased appetite, or body image issues. For many, food restrictions are firmly rooted in OCD, a primary PANS symptom; there are often fears of contamination/poisoning, vomiting, choking, or anaphylaxis. Another symptom of PANS PANDAS is sensory processing issues; hypersensitivity can lead to problems tolerating particular textures, tastes, and smells. Some patients have swallowing issues. Doctors can order a swallowing study if there are obsessional symptoms surrounding vomiting or choking to rule out a physical issue that may be prompting fears. PANS PANDAS patients can have distorted body images, especially in patients who have had PANS PANDAS for several years, so this is seen more often in older patients, but it can happen in younger patients.
PANS patients with restrictive eating may experience significant health issues even if they have not been diagnosed with an eating disorder like Avoidant Restrictive Food Intake Disorder (ARFID) or Anorexia Nervosa (AN). Note that PANS patients with GI issues or stomach pain should discuss causation and treatment with a doctor. Both Lyme and Strep can lead to GI pain, so take care to consider causes.
Increased awareness of eating disorders resulting from PANS is needed to provide proper diagnosis and treatment promptly. Treating PANS/PANDAS is a three-pronged approach: 1) remove the source of inflammation, 2) treat the dysregulated immune system and inflammation 3) treat the symptoms. If PANS patients with eating disorders are not diagnosed correctly, then they are not receiving all three prongs of the PANS PANDAS treatment guidelines; only implementing psycho-therapeutic interventions will not be enough for lasting recovery.

About Restrictive Eating in PANS
- Can include food and fluids
- Reasons
- Sensory processing issues: hypersensitivity to textures, tastes, smells, sounds
- Fears: contamination, poisoning, choking, vomiting, anaphylaxis
- Ritualistic eating behaviors
- Difficulty swallowing
- Decreased appetite
- Body image issues
- Can have a comorbid diagnosis
- Avoidant Restrictive Food Intake Disorder (ARFID) is the diagnosis most seen
- Anorexia Nervosa also possible, though usually PANS patients are not worried about body shape or size, but it is thought this rate increases the longer symptoms persist
- Unlikely to meet the criteria for Binge Eating Disorder (BED) but excessive eating does occur
Importance of Identifying When Restrictive Eating is a Result of PANS

- The therapies for PANS cases are different from those with non-PANS-related ARFID or AN since antibiotics and/or immunomodulatory treatments can be curative. Treatment should consist of the full PANS PANDAS three-pronged treatment approach; treating only psychotherapeutically would more than likely not be sufficient.
- Eating disorder specialist or other targeted therapeutic interventions may be needed in cases of severe symptoms or residual restricted eating
- Restrictive eating can cause malnutrition, nutritional deficiency
- Restrictive eating can cause medical complications
- Restrictive eating can cause significant weight loss or failure to gain weight
- Restrictive eating can cause psychosocial functioning issues & developmental delays
- Restrictive Eating can cause gastrointestinal complications
Restricted Eating Can Lead To
- Nutritionally deficiency
- Significant weight loss or failure to gain weight
- Psychosocial functioning & developmental delays
- Gastrointestinal complications
Risk of Medical Issues Due to Restricted Eating Increase With
- Rapid weight loss
- Significant weight loss in proportion to body size
- Extended periods of restricted eating
- Extreme restriction of fluids or food
Treatment of Restricted Eating Due to PANS PANDAS
Treatment Overview
The duration and severity of restricted eating due to PANS can vary from patient to patient and from flare to flare. PANS PANDAS treatment is dependant on a three-pronged approach: 1-remove the source of inflammation with antimicrobials (if triggered by an infection), 2-treat the dysregulated immune system with immune modulators and/or anti-inflammatories depending on severity, 3-treat symptoms psychotherapeutically as needed. Antibiotics, IVIG, and/or steroids may improve symptoms of bacterial infection-triggered anorexia nervosa quickly. However, patients with continuing eating abnormalities will need medical interventions and psychotherapeutic treatments to focus on factors contributing to the eating restrictions. Patients with insufficient nutrition leading to poor growth or weight loss must be treated aggressively to minimize increased psychological and medical complications. See ASPIRE Treating PANS PANDAS and toolkits for more information on PANS PANDAS treatment.

- Treat PANS PANDAS as per three-pronged PANS treatment recommendations
- Treat the source of inflammation
- Treat the dysregulated immune system
- Focus on maintaining adequate nutrition and hydration while treating underlying brain inflammation
- Medical work up to assess for other medical disorders
- During the acute phases feeding tubes may be necessary
- Feeding Therapy to target factors contributing to ongoing restricted intake
- Exposure and Response Prevention (ERP) for compulsive behaviors and anxiety
- Gradual exposure to situations and food which cause fear in a safe environment
- Incremental progress towards increasing intake and expanding diet
- Cognitive Behavioral Therapy (CBT) to address obsessive, intrusive thoughts
- Occupational Therapy (OT) to address breathing, relaxation, posture may help fear
- Family Therapy to educate and empower families to firmly support goals, to lift blame from the parents and helps build compassion
Medical Work Up for Other Medical Disorders
A thorough medical evaluation should be performed to rule out additional medical disorders due to restricted intake of food and/or fluids.
- Rule out other medical disorders (e.g., eosinophilic esophagitis, structural or neurological causes of dysphagia, and nausea), include a swallowing study if there are fears of choking or vomiting
- Assess for medical instability
- For severely limited intake, assess orthostatic vital signs, EKG, and electrolytes, including phosphorus and magnesium, and monitor for refeeding syndrome
- Hospitalization may be required if medically unstable
Restrictive Eating Cycle
In OCD, there is a loop of obsessive thoughts leading to anxiety that prompts a compulsion, which only provides temporary relief before the intrusive obsessive thoughts dominate again. This vicious cycle is similar to what we may see with restrictive eating restrictions due to PANS. Restrictive eating seen in PANS due to fears, ritualistic behaviors, swallowing issues, or sensory issues may create a vicious cycle. Someone with PANS has their initial reason for avoiding foods or restricting intake, which causes anxiety, then there is temporary relief from not eating, but this reinforces the reasons behind these choices.

Exposure and Response Prevention & Cognitive-Behavioral Therapy
Exposure and Response Prevention (ERP) and Cognitive Behavioral Therapy (CBT) are used in treating ARFID and can be applied to treating patients with PANS PANDAS who have restricted food or fluid intake. ERP may be helpful for compulsive behaviors and anxiety. ERP involves gradual exposure to situations and food which cause fear and anxiety but in a safe and controlled environment. The patient makes incremental progress towards increasing intake and expanding diet. CBT may be helpful to address obsessive, intrusive thoughts. ERP helps remove the fear connected to particular foods. The approach involves rewards for taking small bites of anxiety-inducing food. It also includes talking about and journaling about foods, learning coping skills, and mental visualization. CBT uses talk therapy to help recognize and correct self-destructive patterns of thought and behavior. It can also address other OCD behaviors, anxiety, and depression.

The Goal of CBT/ERP in Feeding Therapy
- Achieve/maintain a healthy weight
- Correct nutritional deficiencies and micronutrient state
- Eat foods from the five basic food groups. Eat a larger range of foods
- Be more comfortable eating in social situations, eating in front of others
- Become less fearful of contamination, choking, or vomiting
- Increase interest in food and eating
The Goal of Treatment is Not
- An attempt to change patient’s personality
- To eat very unusual foods
- To force-feed patients
CBT/ERP Feeding Therapy Outline
- Learn about the disorder and begin to make changes
- Work on determining why food restrictions happen: track situations, triggers, food choices, etc
- Increase intake of preferred foods
- Begin to increase the variety of foods
- Continue to make changes & set goals
- Increase amount of food
- Increase food variety
- Establish goals to face fears
- Begin to face fears, intrusive thoughts
- Begin exposure by starting small and gradually increasing exposure to new foods and exposure to feared foods
- Prevent Relapse
- At the completion of the program, create plans to continue practicing at home to prevent relapse
Family Therapy
Family therapy as used in anorexia nervosa may also be applicable in restricted food intake seen in PANS PANDAS or ARFID. Family therapy focuses on increasing education on the risks of restrictive eating while empowering parents to focus on and be firm about weight gain and nutrition goals. Family therapy also serves to lift blame from the parents and helps build compassion and understanding of the patient’s experience. Families may learn to maintain detailed food diaries and use weight graphs.
Treatment Sources
M Thienemann, T Murphy, J Leckman, R Shaw, K Williams, C Kapphahn, J Frankovich, D Geller, G Bernstein, K Chang, J Elia, S Swedo. JCAP. Sep 2017.566-573. DOI:10.1089/cap.2016.0145
Thomas, J.J. and Eddy, K.T. (2019). Cognitive-Behavioral Therapy for Avoidant/Restrictive Food IntakeDisorder: Children, Adolescents, & Adults. Cambridge: Cambridge University Press.
Wendy Spettigue, MD, Mark L Norris, MD (2019). Understanding and Treating Avoidant Restrictive Food Intake Disorder in Children and Adolescents. Psychiatric Times
PANS & Eating Restrictions at School
Adding Accommodations for Restrictive Eating to an IEP
 One can include accommodations and goals for restrictive eating in an IEP. Feeding therapy is a related service for an IEP as per case law and guidance from OSEP. Feeding therapy support at school is essential if the family does not have a private feeding or cognitive-behavioral therapist. If one has a private therapist, communication between the doctor, therapists, the school, and family is critical. Some families and private feeding therapists may feel that providing support instead of creating goals at school and working on goals outside of school may be more effective. The key is to be consistent in approach. Eating disorders and the therapy can be stressful enough; the addition of other PANS symptoms can be overwhelming. It may be more appropriate to focus on socialization and fun and provide a break during lunch rather than implementing feeding therapy during lunch. Also, it may be more effective to master strategies at home before generalizing to the school environment.
One can include accommodations and goals for restrictive eating in an IEP. Feeding therapy is a related service for an IEP as per case law and guidance from OSEP. Feeding therapy support at school is essential if the family does not have a private feeding or cognitive-behavioral therapist. If one has a private therapist, communication between the doctor, therapists, the school, and family is critical. Some families and private feeding therapists may feel that providing support instead of creating goals at school and working on goals outside of school may be more effective. The key is to be consistent in approach. Eating disorders and the therapy can be stressful enough; the addition of other PANS symptoms can be overwhelming. It may be more appropriate to focus on socialization and fun and provide a break during lunch rather than implementing feeding therapy during lunch. Also, it may be more effective to master strategies at home before generalizing to the school environment.
Eating Restrictions at School PDF
Strategies for School
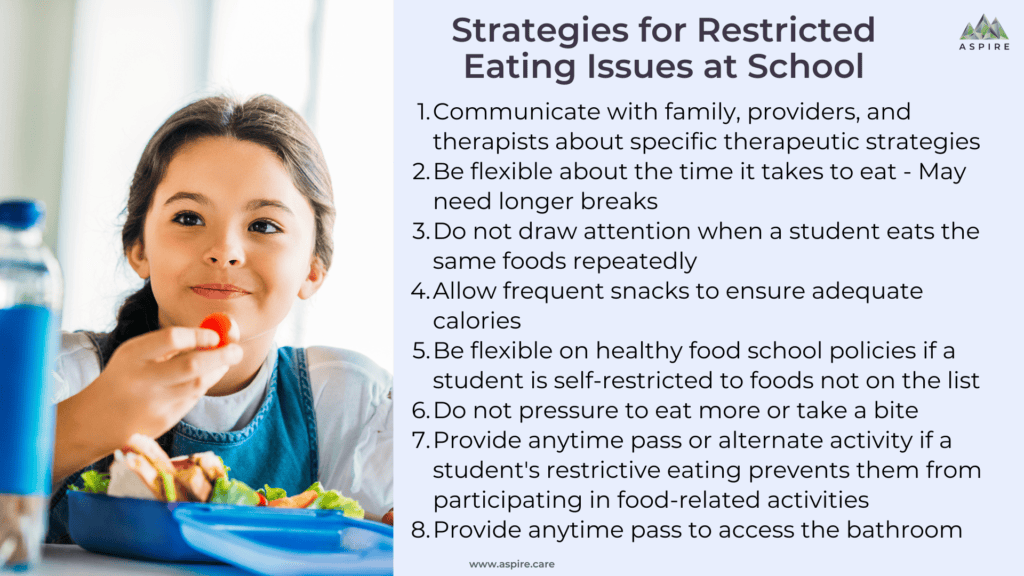
- Communicate with family, providers, and therapists about specific therapeutic strategies
- Be flexible about the time it takes to eat – May need longer breaks
- Do not draw attention when a student eats the same foods repeatedly
- Allow frequent snacks to ensure adequate calories
- Be flexible on healthy food school policies if a student is self-restricted to foods not on the list
- Do not pressure to eat more or take a bite
- Provide anytime pass or alternate activity if a student’s restrictive eating prevents them from participating in food-related activities
- Provide anytime pass to access the bathroom
Relevant Studies
PANS PANDAS Children with Food Restrictions and Disordered Eating (Toufexis Study)

Disordered Eating and Food Restrictions in Children with PANDAS/PANS. Toufexis, DO, et al. JCAP Vol 25, 2015. DOI:10.1089/cap.2014.0063
The rate of eating disorders in children is increasing, especially in males. “Between 1999 and 2006, there was an 119% increase in eating disorder-related hospitalizations for children < 12 years of age.” This increase may be linked to PANS. The authors of the study hope that a PANS diagnosis will be considered in cases with an acute-onset food restriction or avoidance. The therapies and outcomes for PANS cases are different than those with ARFID or AN since antibiotics and/or immunomodulatory treatments can be curative.
The study included 29 children with PANS who had new abrupt onset of eating restriction or food avoidance, ages 5-12 years old.
- 66% fear of contamination (41%-Germs, 10%-Poisoning, 14%-allergens, bleach, illicit drugs, “the essence & personality of other people”
- 28% fear of vomiting
- 21% fear of choking
- 10% body image issues
“In youth with PANDAS, food restriction has been reported to occur in the context of obsessional fears about contamination, as well as in the context of the sudden onset of fears of swallowing, choking, or vomiting that are often associated with sensory phenomena (e.g., the perceived texture or appearance of the food.”
The children in the Toufexis study met the criteria for ARFID. Most “had a paralyzing fear of some adverse consequence of eating normally,” believing they would vomit or choke, and the food was contaminated. The three children, who expressed concerns about “getting fat” or body image, developed those thoughts later.
What is ARFID? “Avoidant and restrictive food intake disorder (ARFID) is a diagnosis in Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (DSM-V) (American Psychiatric Association 2013). Like other DSM-V disorders, the diagnostic criteria for ARFID describe a specific clinical presentation, without regard for etiology, response to treatment, comorbid symptoms, or even acuity of onset.” – Toufexis
Characterization of the pediatric acute-onset neuropsychiatric syndrome phenotype
Murphy TK, Patel PD, McGuire JF, et al. Characterization of the pediatric acute-onset neuropsychiatric syndrome phenotype. J Child Adolesc Psychopharmacol. 2015;25(1):14-25. DOI:10.1089/cap.2014.0062
The study included 43 children with PANS and OCD, ages 4-14 years old.
- 47% had food restriction
- 23% (10) significant impairment related to food restriction (i.e., weight loss, dehydration, and/or hospitalizations), met criteria for ARFID
- 1 had food-related OCD symptoms only
- 9 had OCD symptoms related to food and other issues
- Reason for Food Restriction
- Food-related OCD symptoms included contamination from germs and/or toxins, poison, fear of vomiting, choking
- Fear of weight gain
Use of IVIG for PANS PANDAS
Use of Intravenous Immunoglobulin in the Treatment of Twelve Youths with Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections. Miro Kovacevic, MD, Paul Grant, MD, and Susan E. Swedo, MD – JCAP Vol 25, No 1, 2015 – DOI: 10.1089/cap.2014.0067
Abstract: “This is a case series describing 12 youths treated with intravenous immunoglobulin (IVIG) for pediatric autoimmune neuropsychiatric disorder associated with streptococcal infection (PANDAS). Although it is a clinically based series, the case reports provide new information about the short-term benefits of IVIG therapy, and are the first descriptions of long-term outcome for PANDAS patients.”
Patient A: Patient A was a 7.5-year-old with “initial OCD symptoms included intrusive thoughts, contamination fears (urine, saliva), repetitive compulsive behaviors…, the need to remember what foods she ate looked like, and avoidance of foods she feared she would not remember), and reassurance seeking.” After several treatments including antibiotics, IVIG, steroids and CBT and several relapses, 4 years later she is reportedly doing “very well.”
Patient D: Patient D was a 9.5-year-old boy who “developed a fear of choking and chronic abdominal pain, and the resultant food refusal led to a 4.5 kg (20%) weight loss, hospitalization, and tube feedings. These symptoms persisted for *1 year prior to his evaluation and treatment.” He was given prednisone, IVIG, and prophylactic antibiotics resulting in full remission for a year at the time of follow-up.
Patient G: Patient G was a 9-year-old boy with a history of sudden onset OCD, anxiety, and tics. He later developed more severe sudden onset severe PANS symptoms. “Most significantly, he developed compulsive, recurrent vomiting of all foods and liquids, including water, leading to a 7 kg weight loss. He was diagnosed with postinfectious gastroparesis, and fed exclusively via a nasojejunal tube.” A steroid burst brought temporary improvements. IVIG created dramatic improvement, which allowed him to resume normal food intake orally and the removal of his nasojejunal tube. He did have some residual vomiting, which did not result in weight loss but did interfere with normal life. The second round of IVIG resulted in complete remission. He was still in remission at a three-year follow-up.
Patient L: Patient L was an 8-year-old boy who along with OCD and other PANS symptoms had “a number of ill-defined abdominal complaints that prompted a gastroenterological evaluation (with negative results) and that eventually led to the patient’s complete refusal to eat. The patient lost nearly 25% of his body weight (declining from 22 kg to 17 kg) and was hospitalized numerous times for tube feedings and psychiatric interventions.” Several SSRI’s showed no benefit. Amoxicillin provided a small improvement in symptoms and allowed for stabilization in weight loss. Steroids and IVIG created remarkable improvements and the patient “was able to visit a restaurant (a previously unacceptable venue) and to eat a meal without difficulty.” A second round of IVIG was needed after progress stalled and since recovery has held firm.
Conclusions: This case series demonstrates the benefits of IVIG therapy for youths with PANDAS/PANS, including those who had been symptomatic for several years prior to treatment. Although the generalizability of this retrospective report is limited, the selected cases represent the breadth of symptom presentations in PANDAS/PANS and provide additional evidence that IVIG may be useful in the management of children with moderate-severe symptoms.
Certain Eating Disorders May Be a Neuropsychiatric Manifestation of PANDAS: Case Report
Certain Eating Disorders May Be a Neuropsychiatric Manifestation of PANDAS: Case Report. Cynthia V. Calkin MD; Carlo G. Carandang MD, ABPN (Dip) J Can Acad Child. Adolesc Psychiatry. 2007 Aug; 16(3): 132–135. PMID: 18421369
This case report describes an eight-year-old with PANDAS, OCD, Anorexia Nervosa (AN). “The OCD symptoms were not confined to the Eating Disorder (ED) and the ED symptoms were not exclusively OCD-based.” “This case suggests that EDs, in some cases, may be an autoimmune-mediated neuropsychiatric manifestation or clinical sub-type of PANDAS. The patient in our case rapidly recovered from his ED and OCD. Perhaps by considering the proposed pathophysiology of PANDAS and by targeting the management of future GABHS infections, the usual course of EDs and OCD could be altered in patients believed to have an autoimmune etiology.”
The patient is an eight-year-old boy with “significant weight loss,” behavior changes, and recurrent GAS infections. After being taught healthy eating at school, he began reading food labels and avoiding certain foods. He began looking in the mirror and expressing concerns about his weight. Then he refused to eat his mother’s food as he was distrustful of what she was putting in it. So he only at packaged foods that he determined safe. As a result, he was only eating 200 calories a day. After another strep infection, he developed tics and often did rituals before being able to eat; stating that they, “helps me to relax” and “It distracts me from the images in my head” as intrusive thoughts led him to think that he “must do the hand thing before you eat or the food will poison you” and “your Mommy is a criminal and contaminating your favourite things.” He knew these thoughts were not real, but he was not able to prevent himself from doing them. Additionally, “he developed rules such as having to walk only on his father’s right side so as to not ‘give off (his) fat cells to people walking by.”
“His weight dropped 8kg secondary to his food refusal and he was admitted to hospital at 75% ideal body weight with a score of 33 (extremely severe OCD) on CY-BOCS (Children’s Yale-Brown Obsessive Compulsive Scale) (Scahill et al., 1997)…. It was our opinion that he had PANDAS and he was diagnosed with OCD and AN.” His treatment included re-feeding via an ED protocol, psychiatric medications, one was tolerated while one was not. He received CBT. As he continued to have PANDAS flares, he was given clarithromycin and started to gain weight. “After three weeks of treatment his CY-BOCS score was 19 (moderate OCD) and all choreoform-like movements had ceased. After five weeks of treatment he was no longer having any OCD thoughts and he was not engaging in any ritualistic behaviours.” Once he was at a normal weight, he had a tonsillectomy and has remained stable for 11 months.
Case Study Anorexia Nervosa, OCD & Strep
Anorexia, OCD, and streptococcus. Henry MC, Perlmutter SJ, Swedo SE. J Am Acad Child Adolesc Psychiatry. 1999 Mar; 38(3):228-9. doi: 10.1097/00004583-199903000-00002. PMID: 10087678.
Describes three cases of GABHS-triggered OCD in with obsessional fear of eating. In the first case, the child had typical OCD symptoms followed by a fear of fat contamination, leading to more common AN symptoms. In the second case, a 7-year-old boy had an abrupt onset of fear of eating after choking on pizza. He had a positive throat culture but with no pharyngitis, but antibiotics did not help. Then his OCD included excessive hand-washing and contamination obsessions; behavioral therapy helped. Later, after his sister had positive throat culture, he had an abrupt exacerbation of OCD symptoms. In the third case, a 6-year-old girl, one week after GABHS pharyngitis, developed a fear her food was contaminated. After symptoms did not resolve with an antibiotic, three weeks later, she was hospitalized and improved with sertraline and behavioral therapy. Then she had confirmed strep throat leading to another flare of abrupt contamination obsession. Antibiotics improved symptoms until she had a repeated PANDAS flare.
Case Study Infection-triggered Autoimmune Subtype of AN
Case study: an infection-triggered, autoimmune subtype of anorexia nervosa. Sokol MS, Gray NS. J Am Acad Child Adolesc Psychiatry. 1997 Aug; 36(8):1128-33. DOI: 10.1097/00004583-199708000-00021
The first case describes a 12-year-old boy whose AN worsened one month after an untreated severe upper respiratory tract infection with a negative throat culture but had elevated ASO and anti-DNase-B titers. Antibiotics alleviated his AN. The second case describes a 16-year-old boy who, after a series of URIs, had sudden OCD and failure to gain weight as he grew taller. He had a history of repeated GABHSpharyngitis and had an elevated anti-DNase-B titer. His symptoms resolved after a few months without treatment.
Prevalence of PANS in Child and Adolescent Eating Disorders
 arya Aman, Jennifer Coelho, BoyeeLin, Cynthia Lu, Shannon Zaitsoff, John Best and S. Evelyn StewartBC Children’s Hospital Research Institute, University of British Columbia. See Poster.
arya Aman, Jennifer Coelho, BoyeeLin, Cynthia Lu, Shannon Zaitsoff, John Best and S. Evelyn StewartBC Children’s Hospital Research Institute, University of British Columbia. See Poster.- The surprisingly high lifetime PANS rate of 52% within pediatric ED was higher than that previously reported for OCD populations. The large majority had an abrupt onset of parent-reported OC symptoms as well as abrupt food restriction.
- Those in the PANS group were more likely to be female, be prescribed an SSRI, and have parent-reported abrupt OC symptom onset, abrupt food refusal, relapsing and remitting course, and concurrent anxiety, depression, irritability or aggression, behavioral regression, school deterioration, and sleep problems, enuresis, and/or frequent urination.
- This appears to be a distinct subgroup that requires further characterization with respect to functional impacts and management approaches.”
Anorexia Nervosa Caused by Polymicrobial Tick-Borne Infections: A Case Study
Kinderlehrer DA. Anorexia Nervosa Caused by Polymicrobial Tick-Borne Infections: A Case Study. Int Med Case Rep J. 2021;14:279-287 DOI:10.2147/IMCRJ.S311516
This patient did not have PANS PANDAS but it links Tick-Borne Infections to Anorexia Nervosa.
“Conclusion: There is increasing support for the role of infections in the genesis of AN in some patients. The data suggest that autoimmunity is playing a prominent role in the pathogenesis of microbial-induced AN, and that role has been elucidated in children and adolescents with PANS. This is the first documented case of Lyme borreliosis complicated by three co-infections triggering AN. This adds to the existing literature that infections can play a more prominent role in AN. The corollary is that physicians should become aware of this association in the evaluation of patients with AN, as it may provide a treatment option for this serious and sometimes fatal condition. The possibility that tick-borne infections could underlie the diagnosis of AN warrants further study.”
Obsessive-Compulsive Disorder With Rheumatological and Inflammatory Diseases: A Systematic Review
Alsheikh A M, Alsheikh M M (May 01, 2021) Obsessive-Compulsive Disorder With Rheumatological and Inflammatory Diseases: A Systematic Review. Cureus 13(5): e14791. DOI:10.7759/cureus.14791
This is not about PANS and ED in particular but it is about the link between ED and OCD. Since OCD and Severe Eating Restriction are both major criteria of PANS, we chose to highlight this recent study.
- Difficulties controlling intrusive thoughts is a common symptom between eating disorders and OCD
- Perfectionism symptoms bridge eating disorders and OCD
- Restriction links to checking compulsions and rigidity
- Binge eating links to hoarding symptoms
“The presence of intrusive cognitions and maladaptive perfectionism may contribute to the maintenance of co-occurring ED and OCD symptoms. These findings begin to delineate specific pathways among OCD and ED symptoms, which can be used in the development of interventions to disrupt connections among these disorders.”
Treatment of children and adolescents with avoidant/restrictive food intake disorder: a case series examining the feasibility of family therapy and adjunctive treatment
Spettigue, W., Norris, M.L., Santos, A. et al. Treatment of children and adolescents with avoidant/restrictive food intake disorder: a case series examining the feasibility of family therapy and adjunctive treatments. J Eat Disord 6, 20 (2018). DOI:10.1186/s40337-018-0205-3
“This paper describes six adolescents with ARFID who were successfully treated with a combination of medication plus family therapy, and where indicated, targeted cognitive behavioural therapy. These cases illustrate the complex and various ways in which young patients with ARFID can present, the illness’ effect on development and mental health, and the positive outcomes associated with weight gain and concurrent treatment for co-morbid anxiety disorders.”
Other Eating Disorders
Eating restrictions as a result of PANS PANDAS is not merely picky eating. There are distinct differences between picky eating, ARFID, and Anorexia Nervosa.
About Avoidant Restrictive Food Intake Disorder (ARFID)
ARFID is not just picking eating; it is characterized by restricted food intake due to lack of interest in food, sensory avoidance, or fear of negative consequences. ARFID is different than anorexia nervosa because patients do not worry much about body image or their weight. Patients have underlying biological traits that initially made their eating habits a logical choice, but those food avoidance patterns become longstanding and difficult to change. ARFID was included in the 2013 Diagnostic and Statistical Manual, 5th Edition (DSM-5) as a type of eating disorder. Like other DSM-V disorders, the diagnostic criteria for ARFID describe a specific clinical presentation without regard for etiology, response to treatment, comorbid symptoms, or even acuity of onset. For full criteria, see NEDA. https://www.nationaleatingdisorders.org/learn/by-eating-disorder/arfid
ARFID Presentations
- Lack of interest in eating and food and can get full quickly
- Sensory avoidance leads to issues with food tastes, textures, temperature, and smells
- Fear of negative consequences; fear of choking, allergic reaction, illness, choking
Warning Signs
- Significant weight loss
- Poor weight gain or growth
- Only thinks a few foods are okay, haven’t outgrown picky eating
- Only eating foods with comparable characteristics – color, texture
- Avoids a certain food group
- Gastrointestinal pain
- Nutritionally deficient – seen on lab findings
- Emotional about eating certain foods
- Social situations impacted by food choice constraints
- Difficulty concentrating
- Sleep problems
- Impaired immune function
- Other Physical signs such as
- Dizziness, fainting
- Menstrual irregularities
- Thin hair, brittle nails, dry skin
- Feeling cold
Resources for Eating Restrictions in PANS/PANDAS – Focus on ARFID
About Anorexia Nervosa (AN):
Anorexia nervosa is an eating disorder characterized by weight loss (or gain in children), challenges sustaining a healthy weight, and distorted body image. People with anorexia restrict calories and types of food; they may purge, exercise excessively, or binge eat. One does not have to be underweight to have anorexia. For specific DSM-V information, see NEDA.
- Extreme fear of gaining weight or being overweight
- Extreme restrictive eating leads to significantly low body weight and/or weight loss and inability to maintain nutrition and energy
- Preoccupation with an imagined or slight defect in one’s appearance – disproportionate importance placed on the evaluation of one’s shape or weight or denial of the gravity of too low body weight
Lecture Slides/Recordings/Other Resources
Disordered Eating in Children & Adolescents with PANS. SANE Sweden 2019 PANS Conference Cynthia Kapphahn, MD, MPH, Medical Director-Comprehensive Eating Disorder Program, Clinical Professor, Pediatrics-Division of Adolescent Medicine, Stanford University School of Medicine. Access Slides
Cognitive Behavioral Therapy for Avoidant/Restrictive Food Intake Disorder (CBT-AR): Patient and Family Workbook. Thomas, J.J. and Eddy, K.T. (2019). Cognitive–Behavioral Therapy for Avoidant/Restrictive Food Intake Disorder: Children, Adolescents, & Adults. Cambridge: Cambridge University Press. Access Workbook
How to treat patients with ARFID via telehealth. Jennifer J. Thomas, Ph.D. Eating Disorders Clinical & Research Program, Massachusetts General HospitalDepartment of Psychiatry, Harvard Medical SchoolElissa Chakoff, M.Ed., Ed.S., LMFT, Recovery Record Watch Video & Access Slide
Eating Disorders in the School Context: What School Professionals need to know and what they can do. Tom Bauslaugh, MA, Karen Dixon, MSW, RSWBC Mental Health and Substance Use ServicesProvincial Specialized Eating Disorders Program Access Slides
Books
Please see ASPIRE’s Book section.
Other Handouts on PANS & Eating Restrictions
PANS and Restricted Eating Awareness flyer (available to download in poster sizes). Several ASPIRE PANS PANDAS fliers are available for you to print in three sizes, one letter-size paper, and two poster sizes. The .pdf version below is an 8.5×11 paper size. If you would like the 11×14 or 16×20 poster version for you to download and print for an event, please contact Gabriella True directly so we can know about your event and help promote it.
Restrictive Eating at School flyer Please also see ASPIRE PANS in the School Setting website section with toolkit and School Nurse Role website section with toolkit.
PANS & Restrictive Eating Flyer & Poster
Return to Section:



One comment to PANS & Eating Disorder/Food Restrictions & Toolkits/Handouts
Ufed Treatment
February 21, 2024Your blog provided us with valuable information to work with. Each & every tips of your post are awesome. Thanks a lot for sharing