Toolkit – PANS/PANDAS Guidelines for Children with Autism
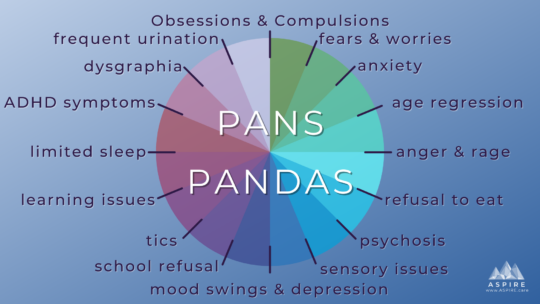
ASPIRE’S Professional Advisory Board publishes PANS/PANDAS Guidelines for Children with Autism PANS PANDAS & Autism Autism PANS Guidelines Children who have autism spectrum disorder (ASD or...





 PANS PANDAS Clinician Toolkit
PANS PANDAS Clinician Toolkit
 PANS PANDAS Guidelines for Children with Autism
PANS PANDAS Guidelines for Children with Autism