Fifteen Years Misdiagnosed: My PANS Journey
⚠️ Trigger Warning: This story contains references to self-harm, suicidal thoughts, and substance use. Mature audiences only. ⚠️ A young adult endured years of psychiatric hospitalizations,...
⚠️ Trigger Warning: This story contains references to self-harm, suicidal thoughts, and substance use. Mature audiences only. ⚠️ A young adult endured years of psychiatric hospitalizations,...
Strep throat is a common childhood illness, but in a few children this bacteria infection can lead to alarming, lasting changes in behaviour. Scientists are now starting to unravel how it affects the...

Current Legislative Action Please visit the MI PANS/PANDAS Alliance to stay updated on how you can take legislative action in Michigan. If you are a Michigan parent of a...
Joint Rebuttal to the American Academy of Pediatrics Clinical Report on PANS (12/16/24)...
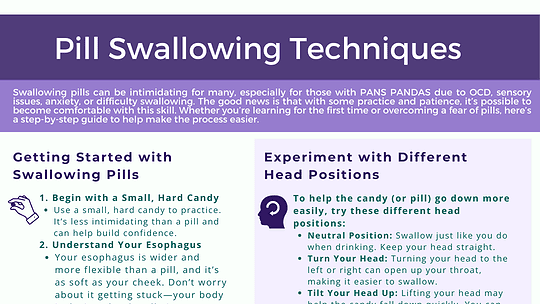
Swallowing pills can be intimidating for many, especially for those with PANS PANDAS due to OCD, sensory issues, anxiety, or difficulty swallowing. The good news is that with some practice...

🌿 In May, during Mental Health Awareness Month, our Nebraska State Leads—Grace Troupe and Elizabeth Fandl—joined Where There’s a Will Foundation for their annual mental health awareness walk...
Sonbol, H.M., Abdelmawgoud, A.S., El-kady, N.M. et al. Serum zonulin level in autistic children and its relation to severity of symptoms a case-control study. Sci Rep 15, 27802 (2025). https://doi.org/10.1038/s41598-025-11420-0

Virginia PANS PANDAS Updates Virginia Alliance for PANS/PANDAS Action (VA4PA) is leading legislative efforts. Please contact them directly for more information. Their website is VA4PA and...
Han VX, Alshammery S, Keating BA, Gloss BS, Hofer MJ, Graham ME, Aryamanesh N, Marshall LL, Yuan S, Maple-Brown E, Yan J, Bandodkar S, Kothur K, Nishida H, Jones H, Tsang E, Lau X, Dissanayake R, Perkes I, Mohammad SS, Brilot F, Gold W, Patel S, Dale RC, et al. Epigenetic, ribosomal, and immune dysregulation in paediatric acute-onset neuropsychiatric syndrome. Molecular Psychiatry. 2025;30:5389–5404. doi:10.1038/s41380-025-03127-5
Compared children with PANS and other neurodevelopmental disorders to neurotypical controls; PANS/non-PANS groups reported more early childhood infections and loss of previously acquired developmental skills than controls.
Found routine immune testing largely normal, but RNA sequencing showed upregulated ribosomal biogenesis/RNA methyltransferase pathways and downregulated mitochondrial, signaling, endocytosis, and immune pathways.
Toll-like receptor stimulation showed reduced TNF and IL-6 responses in PANS; post-IVIG RNA sequencing demonstrated partial normalization of dysregulated pathways.
Authors conclude findings support immune and epigenetic dysregulation in PANS and provide rationale for immune-modulating therapies.
Turowski, P., Fetz, K., Chang, K. et al. Pediatric acute neuropsychiatric syndrome (PANS) and Pediatric Autoimmune Neuropsychiatric Disorders associated with Streptococcal Infections (PANDAS) in the Context of EMTICS: Methodological Considerations and Misinterpretations. Eur Child Adolesc Psychiatry 34, 3685–3688 (2025). https://doi.org/10.1007/s00787-025-02747-0
“With the identification of biological markers, distinctions between syndromes like PANS and PANDAS may become clinically obsolete, shifting focus to underlying mechanisms rather than clinical presentation.” The authors argue that current labels like PANS and PANDAS are largely symptom-based frameworks that exist because we lack definitive biological tests. As research identifies reliable biomarkers such as immune signatures, autoantibodies, or inflammatory pathways, these distinctions may become less clinically relevant. Instead of categorizing patients by how symptoms present or which trigger is suspected, diagnosis and treatment could shift toward the underlying biological mechanisms driving illness, allowing for more precise, mechanism-based care rather than reliance on descriptive clinical syndromes.
It’s one of the more common illnesses: strep throat. According to the Centers for Disease Control, strep throat is now at a 20-year high. It is a bacterial infection in your throat and tonsils,...