Thank You for an Incredible Awareness Day!
I want to thank our entire community for participating in PANS PANDAS Awareness Day yesterday. Your posts, lights, and conversations made a powerful impact. Today is World Mental Health Day,...
I want to thank our entire community for participating in PANS PANDAS Awareness Day yesterday. Your posts, lights, and conversations made a powerful impact. Today is World Mental Health Day,...
Weinstock LB, Afrin LB, Reiersen AM, Brook J, Blitshteyn S, Ehrlich G, Schofield JR, Kinsella L, Kaufman D, Dempsey T, Molderings GJ. Prevalence and treatment response of neuropsychiatric disorders in mast cell activation syndrome. Brain, Behavior, & Immunity – Health. 2025;48:101048.doi:10.1016/j.bbih.2025.101048
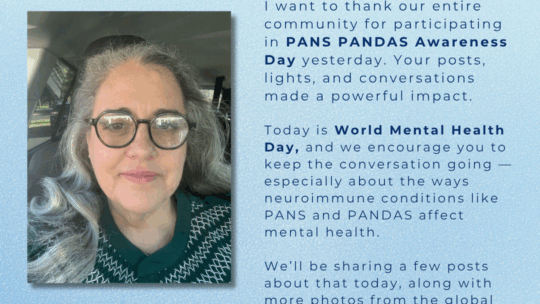
Daily Herald – Suburban Chicago’s News Source October 06, 2025 On Thursday, Oct. 9, the Millennium Carillon in Naperville will light up green in honor of World PANS/PANDAS Awareness Day,...
By Gabriella True, President, Alliance to Solve PANS & Immune-Related Encephalopathies (ASPIRE) Each year, countless children and adults with PANS PANDAS lose critical time, time when early...

Volunteers Needed: We need volunteers to reach out to their municipalities to request that they light up monuments, like the state house, bridges, monuments, etc., be lit up on October 9th,...
When Inflammation Is Dismissed: B’s Battle with PANS and Tick-Borne Co-Infections Acute neuroinflammation can be life-changing—and it’s appalling when providers dismiss these symptoms as...

When severe food restriction and complex symptoms are mistaken for FND, proper evaluation is crucial. When Sophie got the flu at age 12, she didn’t expect it would mark the...
When a child’s behavior changes dramatically overnight, early recognition can make all the difference. This 6-year-old daughter woke up with sudden, severe contamination OCD, separation anxiety,...
When your child declines rapidly and no one believes you—trusting your instincts can save the day. Countless calls to pediatricians and child psychologists led nowhere. No one believed her symptoms...
McKenzie hasn't officially been diagnosed with PANDAS by her pediatrician, as we are in the early stages; however, no one can convince me otherwise. My family's life has been completely turned upside...

One year ago, Penelope was bitten by a tick, marking the beginning of our journey to uncover the truth. When she showed me the characteristic bull's-eye bite, I initially mistook it for a spider...
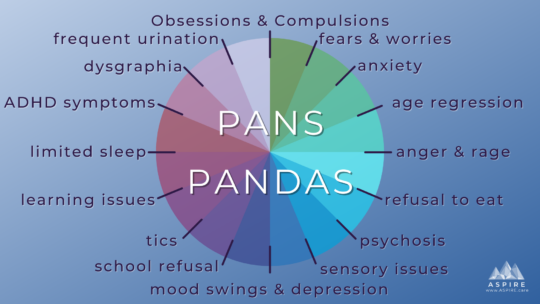
Learn more about PANS PANDAS PANS PANDAS are misdirected immune responses that result in acute onset of OCD, tics, and/or restricted food intake, along with two neuropsychiatric symptoms in seven...