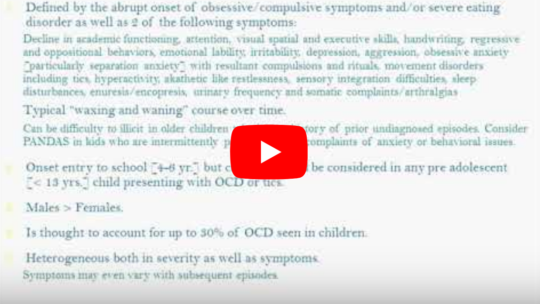
MCPAP – Pediatric Neuropsychiatric Disorders (Associated with Streptococcus): PANDAS/PANS
Presented by: Michele Casoli-Reardon, MD, MCPAP North Shore Medical Center Team Medical...
Presented by: Michele Casoli-Reardon, MD, MCPAP North Shore Medical Center Team Medical...

There’s nothing black and white about this mysterious and controversial diagnosis. If your child suffers sudden mental health problems following a case of strep throat, this autoimmune condition...

This video describes the Cunningham Panel of tests and explains the value of and symptoms associated with each of the assays. The role of Dopamine 1, Dopamine 2, Tubulin, Lysoganglioside GM2 and CaM...
This case report describes the effective use of Saccharomyces boulardii in a boy with autism spectrum disorder, obsessive compulsive disorder (OCD), and self-injurious behavior (SIB). Gastrointestinal dysfunction and OCD are frequent comorbidities in autism, which may share a common etiology resulting from a disturbance in normal gut microbiota. Alterations in microbial diversity influence neuroinflammation and are linked to mood disorders, abdominal pain, and SIB. S boulardii is a nonpathogenic probiotic yeast that supports a healthy microbiome, enhances immune function, and reduces diarrhea. Treatment with S boulardii successfully reduced OCD and SIB symptoms in this child.

Steele Center University of Arizona – CPAE Center of...
What PANS, PANDAS, and Autoimmune Encephalitis are and why so many children are being diagnosed with these conditions.• What causes PANS.• Why PANS is so commonly seen in children with...
Melanie Uhde, Alyssa Indart, Brian A Fallon, Gary P Wormser, Adriana R Marques, Suzanne D Vernon, Armin Alaedini, C-Reactive Protein Response in Patients With Post-Treatment Lyme Disease Symptoms Versus Those With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, Clinical Infectious Diseases, Volume 67, Issue 8, 15 October 2018, Pages 1309–1310, https://doi.org/10.1093/cid/ciy299
In honor of PANS/PANDAS Awareness Day 2018, I am here with a panel of mama and a papa heroes, who have children with PANS to help me spread the awareness...

One afternoon in the winter of 2017, Corie Entrop’s 10-year-old son came home from school and began pulling out his hair. When the Alberta mother pleaded with him to tell her why he was doing it,...

Moving Past Controversy to Provide Clinical...

PANDAS/PANS Standards of Care Summit October 4, 2018 State Fairgrounds, Springfield...