Posts found in:
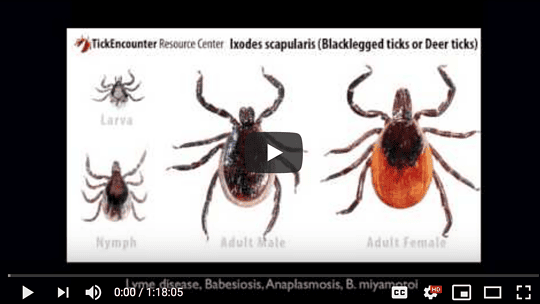
Lyme Disease
An Osteopathic Approach to Lyme Disease – Dr. Thomas A. Moorcroft, DO
Dr. Moorcroft discusses an Osteopathic approach to Lyme Disease & Tick-borne Co-infections at the 2016 Lyme Conference at Binghamton University, Co-hosted by Southern Tier Lyme Support, Inc....

Dr. Geordie Thompson – NEPANS – NH Conference 2015
A fantastic overview of Lyme disease. This presentation covers Lyme as it exists, and how it can effect those with a PANS/PANDAS...

When Your Child Has Lyme Disease: A Parent’s Survival Guide
When Your Child Has Lyme Disease: A Parent's Survival Guide is filled with information parents need to know about Lyme, as well as practical strategies based on the authors' personal and professional...

PANS and Lyme Disease in ASD – Tracy Fritz, MD
Dr. Fritz will discuss signs and symptoms of PANS/Lyme and appropriate evaluation and treatment, including natural and pharmaceutical antimicrobials, immune modulating therapy, and an integrative...
Increased IFNα Activity and Differential Antibody Response in Patients with a History of Lyme Disease and Persistent Cognitive Deficits
Lyme disease and pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS): an overview
Rhee H, Cameron D. Lyme disease and pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS): an overview. Int J Gen Med. 2012;5:163-174
https://doi.org/10.2147/IJGM.S24212
B. burgdorferi and GAβHS are very different microorganisms that evade the immune system and invade a wide variety of tissues, including the central nervous system (CNS). Lyme and PANS can have periods of active disease and periods of remission. Both infections cause physical, neurological, and cognitive symptoms.
The neuropsychiatric manifestations of Lyme borreliosis
Borrelia burgdorferi in the nervous system: the new “great imitator”
Pachner AR. Borrelia burgdorferi in the nervous system: the new “great imitator”. Ann N Y Acad Sci. 1988;539:56-64. doi: 10.1111/j.1749-6632.1988.tb31838.x. PMID: 3190104.
Patient Vignette – Bicycle Boy
The patient was bitten by a tic. Weeks later he presented with neuropsychiatric symptoms. Was given IV antibiotics and all symptoms resolved.
Clinical and diagnostic manifestations of tickborne mixed infection in combination with COVID-19
- The study investigated the coexistence of pathogens in a patient, focusing on the relationship between laboratory diagnostics and clinical manifestations during SARS-CoV-2 infection in a case of chronic encephalitis-borreliosis.
- Blood samples collected over a year revealed Lyme disease diagnosed through IgG antibodies to Borrelia, with joint pain and erythema migrans. Subsequently, the patient contracted SARS-CoV-2 during a Lyme disease exacerbation.
- Treatment improved the underlying disease but led to TBEV activation, possibly due to immune system focus on SARS-CoV-2. Despite TBEV activation, clinical manifestations were absent, suggesting weak virulence. Etiotropic treatment suppressing borreliosis led to TBEV activation, highlighting the dominance of B. burgdorferi in tick-borne infections.